A recent study reported that medical error is the third-leading cause of death in the United States, just ahead of respiratory illness and behind only cardiac disease and cancer.1 More than 200,000 American deaths each year are associated with preventable harm in hospitals.2 In addition to putting patients at risk, medical errors contribute to substantial avoidable costs estimated to exceed $17 billion annually in direct costs in the U.S. alone.3 Given that up to 70 percent of clinician decisions are influenced by laboratory test results, there is a major role for the clinical laboratory to play in reducing avoidable medical error, enhancing patient safety, and improving outcomes.4
Lab error and patient safety
The ECRI Institute publishes an annual report on the Top 10 Patient Safety concerns. In the most recent report, two of the top ten, “test result reporting and follow-up,” and “patient identification errors,” are directly related to issues that can be addressed by the clinical laboratory.5 Patient identification errors and test result reporting are associated with the pre-analytical and post-analytical stages of clinical diagnostic testing.
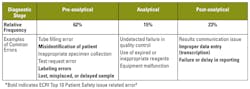
And while recent studies have shown that errors occur across all three stages of the diagnostic process, up to 62 percent of the diagnostic errors occur in the pre-analytical stage and up to 23 percent in the post-analytical stage (Table 1).6,7 Outstanding analytical performance remains a critical consideration for laboratories, but tools that can help address the majority of laboratory-related errors that occur in the pre- and post-analytical stages are of growing importance to laboratory leaders.
Regulators of laboratory quality standards are also taking steps to help address laboratory-related medical errors and patient safety risks. The Joint Commission, Clinical Laboratory Improvement Amendments (CLIA), and College of American Pathologists (CAP) are increasing their quality standards for laboratory accreditation and compliance with revisions to Conditions of Participation, which can impact payments from the Centers for Medicare and Medicaid Services.8
There is also increasing awareness of medical error among patients. As part of the movement toward more consumer-driven healthcare, organizations such as Leapfrog Hospital Safety Grade Ratings are collecting and reporting on patient safety measures that empower patients with information that enables them to choose where they seek care.
This growing body of research on laboratory error sources and emphasis on patient safety creates a challenge for laboratory management to address while at the same time juggling shrinking budgets and personnel constraints.
Automation and safety goals
Laboratory automation can improve patient safety and help labs achieve their safety goals. Clinical labs have benefited from the advent of new technologies and instruments over the last decade. Notably, lab automation has expanded beyond the chemistry lab and moved into virology and microbiology with the growing adoption of fully automated robotics and sample-to-answer molecular platforms designed to remove the most complex and error-prone steps of the diagnostic testing process. While these sample-to-answer platforms have provided significant operational benefits in the lab, opportunities remain to further improve the pre- and post-analytical workflow of these platforms in order to address patient safety concerns.
Reducing the complexity of pre-analytical workflow steps has been a focus of more recent molecular diagnostic sample-to-answer systems which emphasize the importance of an intuitive and easy-to-use workflow in the laboratory. These systems have provided an opportunity to reduce pre-analytical errors by taking complex, multi-step procedures for sample extraction, amplification, and detection and consolidating them onto a single platform where sample preparation and loading requires fewer than five steps. Lab staff also benefit by the reduction of complex manual steps and those that require repetitive motion or the use of manual force, which can contribute to operator fatigue and repetitive strain injuries (e.g., carpal tunnel syndrome and tendonitis). Platforms with usability engineering-based designs will enable laboratorian interactions in a proper posture, aiding in ease of use, comfort, and injury prevention. Fewer hands-on steps and less physical strain and fatigue can help reduce the risk of avoidable error in the pre-analytical stage.
Bi-directional instrument interfaces
Lost, misplaced, or delayed patient samples can contribute to delayed diagnosis and treatment. One solution that addresses these challenges is a bi-directional interface with the laboratory information system (LIS). Automating the process of downloading and tracking pending test orders combined with user-configured notifications can help laboratorians proactively identify potentially lost, misplaced, or delayed samples. Lab automation can also assist with sample stability tracking by identifying samples that have exceeded the pre-set stability time from collection and alert the appropriate lab staff, thus avoiding processing samples which could generate an inaccurate result.
Sample identification and tracking limitations of prior generation systems have historically created an opportunity for avoidable error in the lab. For example, sample mismatch errors are one of the more common failure modes during the pre-analytical testing process. Platforms designed with a testing consumable that has adequate space to place a patient/accession barcode directly on the consumable eliminate the need for hand-written patient identifiers and can greatly decrease the chance of sample mismatch errors. The risk of sample mismatch can be further reduced by automated chain-of-custody and process controls to ensure the patient scanned is the patient tested, a capability commonly referred to as positive sample identification (PosID). PosID features are highly advantageous along the entire testing process to ensure that the primary patient sample matches the result reported to the physician.
Analytical and post-analytical risks
While analytical errors represent the smallest percentage of diagnostic errors, vendors can design platforms with features that further reduce this type of error. A common analytical phase risk is the use of expired reagents or testing patient samples on reagents that have not passed quality control (QC) inspection. Not only can these errors lead to an inaccurate patient result; they can also result in non-conformances during laboratory inspections by CLIA and CAP. Advanced diagnostic platforms aid in ensuring compliance by providing automated software features to prevent the use of expired reagents and to track external QC. These systems also provide lab-configured notifications to remind staff that an external QC time point is approaching, thus preventing patient sample testing if QC is past due and ensuring patient testing is never delayed to accommodate QC. Sophisticated software features and embedded process controls that automatically identify analytical failure modes can reduce reliance on human vigilance alone and help ensure critical steps are not inadvertently overlooked by busy laboratory staff.
Post-analytical failure modes are often attributable to data entry errors during manual transcription of results to the LIS and delays in results reporting when the diagnostic platform does not support full LIS interface capabilities. Implementing LIS-ready platforms in the laboratory eliminates data entry transcription errors by automatically releasing results directly to the LIS. Platforms that enable rules-based auto-verify functionality can be configured to automatically send specific results to the LIS and reduce sample turnaround time, as laboratorians are not required to return to the instrument after test completion to manually release results to the LIS. Delivering rapid order-to-report turnaround time enables faster clinical actions, which has been shown to lead to improved patient outcomes in a number of settings. This level of platform sophistication in the clinical laboratory will be commonplace in the coming years to positively impact patient safety by reducing turnaround time and transcription errors.
The view from here
Significant progress has been made on the issue of avoidable medical error since the Institute of Medicine’s groundbreaking publication of To Err is Human almost 20 years ago.9 Yet many challenges remain, among them the fact that the true number of laboratory errors is unknown and likely underestimated, as many go undetected or their impact is confounded by other interventions in the patient care pathway. The risks associated with these errors can be reduced by leveraging automation, software features, and user-centered system design. This system design approach will not only benefit patients but also help improve laboratory efficiency and engagement by allowing skilled staff members to focus on the highest value activities in the lab. Public disclosure and market pressures are helping to create awareness of hospital quality and drive institutional metrics to improve patient safety and satisfaction. Continued advances in lab automation and platforms with patient safety as a core design element will increasingly contribute to delivering on the shared goal of delivering high value, patient-centered care.
REFERENCES
- Daniel M, Makary M. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139.
- James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Safety. 2103;9(3):122–128.
- Van Den Bos J, Rustagi K, Gray T, Halford M,Ziemkiewicz E, and Shreve J. The $17.1 billion problem: the annual cost of measurable medical errors. Health Affairs. 2011;30(4):596-603.
- Forsman RW. Why is the laboratory an afterthought for managed care organizations? Clin Chem. 1996; 42(5):813-816.
- ECRI Institute Names Top 10 Patient Safety Concerns for 2017. https://www.ecri.org/press/Pages/Top-10-Patient-Safety-Concerns-for-2017.aspx. Published March 13, 2017.
- Carraro P, Plebani M. Errors in a stat laboratory: types and frequencies 10 years later. Clin Chem 2007;53(7):1338-1342.
- Wians, Frank H. Clinical laboratory tests: which, why, and what do the results mean? Lab Med.2009:40(2)105-113.
- College of American Pathologists. CAP Releases 2017 Laboratory Accreditation Checklists With Detailed Requirements to Improve Laboratory Quality. http://www.cap.org/web/submenu/news/press-releases/press-release?contentID=1-142376&_adf.ctrl-state=11swpmjgij_75&_afrLoop=409078222000694#!%40%40%3F_afrLoop%3D409078222000694%26contentID%3D1-142376%26_adf.ctrl-state%3Dhbszuomuj_4.
- Kohn L, Corrigan J, Donaldson M. To Err is Human: Building a Safer Health System. Washington Institute of Medicine, National Academy Press, 2000.
Brad F. Tieman, MBA, serves as Director of Marketing for San Diego-based GenMark Diagnostics.