A system-wide movement to improve patient care and reduce unnecessary laboratory testing
A grassroots movement initiated by phlebotomists began a revolution at Lawrence General Hospital (LGH) in Lawrence, Massachusetts. These healthcare team members championed the cause of patients and staff who had reported unnecessary lab testing. Their dedication to patient care led to a hospital-wide procedural change. This article identifies a common problem affecting many hospitals adversely, our process of change management at LGH, and the subsequent improvement in both laboratory utilization and cost-reduction outcomes.
Relevant background and context
In July 2014, LGH’s Lab Utilization Committee (LUC) formed the Duplicate Order Task Force to address a concern that had been raised by members of the phlebotomy team. Phlebotomists had observed that there were many duplicate lab order requests, resulting in excessive blood draws and numerous patient complaints.
LGH staff knew that excessive blood draws and adverse patient outcomes were problems that were far from unique to their institution. One published survey of 17,676 patients in 57 United States hospitals from 2000 to 2008 showed that 20 percent of patients who didn’t have anemia when admitted for heart attacks developed moderate to severe cases of the red blood-cell deficiency by the time they left.1 The average volume of blood drawn from patients who developed anemia was 174 milliliters (more than double the 83.5 milliliters from patients who didn’t develop anemia). For every 50 milliliters of blood drawn, risk of moderate to severe hospital-acquired anemia increased by 18 percent. The average blood loss across hospitals ranged from 119 to 246 milliliters, indicating that some blood loss could be prevented by eliminating routine testing. Moderate to severe hospital-acquired anemia is independently associated with higher in-hospital mortality in patients with myocardial infarction.2
Risk Management at LGH received 512 formal incident reports in a three-month span. This observation surfaced during a crucial period in LGH history. Six months prior, the labs’ ordering practice had changed from laboratory information system (LIS) to hospital information system (HIS). The LIS had built-in logic to prevent duplicate order placement. When the HIS launched live, no internal system existed to alert duplicate orders. Hospitalists, primary care providers, and specialists were ordering the same labs, as there were no alerts in the computerized physician order entry system (CPOE). Daily repeat labs were ordered, such as international normalized ratio (INR) for patients on warfarin and basic metabolic panels (BMP) to follow creatine for patients with acute kidney injury. Patients were subject to multiple draws of the same tests on the same day.
As the multidisciplinary team gathered support for prevention of duplicate and daily blood testing, there was a strong contingent of physicians who opposed this project. The previous physician culture was reluctant to implement systemic changes to prevent duplicate testing. However, after several meetings with the Utilization Review Committee and the Medical Executive Committee, it became clear that removal of duplicate orders was the appropriate action for patients.
CPOE has many proven benefits, such as reduction of illegible hand written orders,3 optimization of clinical time, and streamlining of communication between clinicians and other departments.4 However, there was an obvious disconnect in the quality of patient care. This problem led to utilization of Clinical Decision Support (CDS) alerts and an alert system embedded in CPOE (Figure 1). Studies demonstrate that CDS alerts led to reduction of medical errors and quality of care improvement.5 It is important to note that overuse of diagnostic laboratory tests is in fact identified as medical error.5 The reduction of medical error can have significant impacts on cost reduction. The Triple Aim6,7—better care for lower costs and better patient experiences— is certainly a goal at LGH, and the introduction of CDS is one example of a strategy designed to meet that goal.
Process and outcomes of change
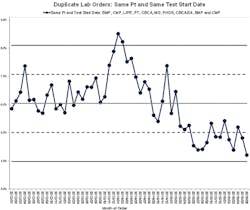
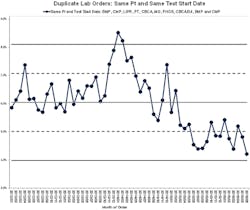
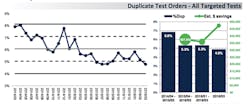
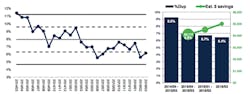
A multidisciplinary team assembled to move toward the goal of reduced duplicate orders. Figure 1 highlights the top duplicate order tests. The associated fiscal savings are shown in Figure 2. The peak of lab ordering occurred in December 2013, which coincided with the launching of CPOE. Data was collected over a four-year period from January 2012 to June 2016. A three percent decrease was demonstrated for the following orders: basic metabolic panel (Figure 3), comprehensive metabolic panel, complete blood count, prothrombin time, phosphorous, magnesium, international normalized ratio, lipids, and troponin. This reduction of ordering was achieved by CDS alerts. The projected savings from this intervention is $37,542. Furthermore, CPOE was modified with removal of daily esoteric testing and a three-day consecutive test max for the top six assays. The savings, fiscal year to date, amounted to $83,500.
The Duplicate Order Task Force utilized CDS to promote key tenets of population health: improved patient experience, quality with fewer adverse events,6 and significant cost reduction. CDS has been studied to show improvement of clinician performance in lab ordering via the following measures: display of cost of the lab order, display of previous test results, use of reminders, and display of recommendations.4 LGH saw a gradual shift in culture from reactive to proactive measures to foster patient health and wellness. Reduction of waste led to a gain in efficiency and increased patient satisfaction. Financial performance grew stronger as the process of care delivery trimmed out unnecessary measures. The endpoint for LGH and our project is the delivery of evidence-based care and adherence to best practice, which helped our institution achieve the Triple Aim.
The reduction in unnecessary utilization of lab resources is an enabling factor to the lab bottom line as an outpatient revenue center. The lab is meeting increased outpatient demand without matching increases in cost. Fewer inpatient orders and better utilization has increased our capacity to do more outpatient lab tests, which is fee-for-service. CDS embedded into CPOE frees lab personnel to complete other value-added tasks rather than manually sifting through duplicate order sets, thus furthering the opportunity for better utilization of lab staff time.
Better safety and satisfaction
In summary, CDS implementation in CPOE reduced unnecessary lab utilization without a single reported adverse event. Sustainable healthcare systems are founded in quality of care and reduction of cost and medical error. As such, proper resource utilization is essential to move forward in the climate of healthcare reform. The success of this project is a testament to the value of coordinated team care and a multidisciplinary approach. A multidisciplinary support for the Lab Utilization Committee enabled the Duplicate Order Task Force to reach out to other hospital committees and departments to facilitate a transferrable workflow change. In the case of duplicate orders, less proved to be more and change moved forward as a collaborative effort. The ripple effects of this project led to multi-department changes at LGH in MRI services, CT Scans, and Pharmacy.
REFERENCES
- Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171(18):1646-1653.
- Salisbury AC, Amin AP, Reid KJ, et al. Hospital-acquired anemia and in-hospital mortality in patients with acute myocardial infarction. Amer Heart J. 2011;162(2): 300 – 309.e3.
- Bates DW, Leape LL, Cullen DJ, et al. Effect of Computerized Physician Order Entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280(15):1311-1316.
- Main C, Moxham T, Wyatt JC, Kay J, Anderson R, Stein K. Computerised decision support systems in order communication for diagnostic, screening or monitoring test ordering: systematic reviews of the effects and cost-effectiveness of systems. Health Technol Assess. 2010;14(48).
- Levick DL, Stern G, Meyerhoefer CD, Levick A, Pucklavage D. Reducing unnecessary testing a CPOE system through implementation of a targeted CDS intervention. BMC Medical Informatics and Decision Making. 2013 13:43.
- Nash DB, Fabius RJ, Skoufalos A, Clarke J, Horowitz MR. Population Health: Creating a Culture of Wellness. 2nd ed.
- Berwick DM, Nolan TW, Whittington J. The Triple Aim: Care, health, and cost. Health Affairs. 2008;27(3):759-769.
Pracha Eamranond, MD, MPH, is Assistant Professor at Harvard Medical School and Senior Vice President of Medical Affairs and Population Health at Lawrence General Hospital (LGH). Megha Joshi, MD, is Chief of Pathology and Medical Director at LGH. Insha Haque, DO, is a second-year resident physician at NH Dartmouth Family Medicine Residency and Population Health Extern at LGH. Alison Scarry, MS, H, BB(ASCP), serves as Administrative Laboratory Director at LGH. Stephan Geary, MLS(ASCP)SH, is a Core Lab Supervisor at LGH. Brian Collins, BS, serves as Director of Decision Support at LGH.