The laboratory’s contribution to advanced medical analytics
The laboratory represents only about three percent of healthcare costs, but when it is used properly, it can impact downstream costs far beyond the cost of performing lab tests. As healthcare moves into the future, proactive, preventive, and patient-focused care will require new innovations and a fresh perspective. Laboratorians are encouraged to see the value of the information they are processing and to become active participants in analytics that advance the value of lab information.
If you shut down labs, you shut down healthcare
In response to the continual threat of reduced lab reimbursements, one of the keynote speakers at the 2015 Lab Quality Confab, John Waugh, MS, MT(ASCP), of Henry Ford Health Systems, presented the question, “What if we shut down ALL laboratories?” He displayed an excerpt from “The Waugh Street Journal” (Figure 1).
His humorous parody of a Wall Street Journal article makes two excellent points that laboratorians should take heed of: 1) If labs shut down, healthcare shuts down; and, 2) Of the $3.2 trillion healthcare spending bill, the lab accounts for a very miniscule portion. However, while the lab is not the problem in rising healthcare costs, it can be a huge part of the solution. Providers cannot take care of patients without the lab, so the lab will not go away as a tool in healthcare. In fact, it is just the opposite; the lab actually becomes more valuable. Because lab testing is healthcare’s highest-volume activity, providers rely heavily on laboratory data.
Labs will remain, but where they remain will be a question of cost and value. Labs remain essential no matter what happens to reimbursements. Yet what will change is which labs are successful and which facilities decide to outsource lab testing. This will come down to the level of value provided by the specific laboratory; and analytics can play a substantial role in demonstrating a lab’s value. Laboratory-driven analytics projects not only demonstrate lab value, but can actually drive down costs and support care improvements.
The lab is the hub of diagnostics
The changes taking place in healthcare offer great opportunity for the lab because the lab sits on the hub of clinical data that feeds diagnostic decision-making—information that will change the way we deliver and pay for care. The transition to value-based reimbursements is requiring providers to use quantitative metrics to justify quality and associated
reimbursements.
For example, healthcare organizations within an Accountable Care Organization (ACO) must track a multitude of measures to establish quality performance standards in order to achieve shared savings. There are interactions between ACO quality reporting and other CMS initiatives, such as the Physician Quality Reporting System (PQRS) and the Meaningful Use EHR Incentive Program.1 Patient-centered Medical Homes use the Healthcare Effectiveness Data and Information Set (HEDIS) to track performance.2
In addition to required performance measures, healthcare data is being used to glean actionable knowledge to drive decisions regarding patient care and find ways to reduce healthcare spending. The shifts we are seeing in healthcare reimbursement and the new methodologies for tracking quality will only substantiate the laboratory as an even more valuable part of the patient care plan. How can the lab, which holds the bulk of the clinical information, be more involved in gaining value from their data?
Internal views: a fresh perspective on data analytics
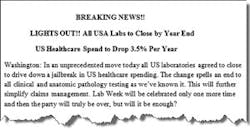
Laboratories are already known for their efficiency and focus on reporting quality results, and are accustomed to being on a tight budget. Now it is time to branch out beyond those mastered areas and make a bigger impact. To take this to the next level, labs can use internal analytics to support the ordering provider by offering expertise in test order optimization and interpretation. This can involve one of many interventions, from offering duplicate test alerts or testing cascades at the time of Computerized Physician Order Entry (CPOE), to using variation analysis studies, test formularies, or comprehensive test utilization plans to reduce waste and promote best orders. Additionally, analytics can be used to pursue a Lean culture by tracking staffing to workload, inventory control, and monitoring turnaround times (TATs) (Figure 2).
External impact: increasing the lab’s effectiveness
Lab value comes from results that drive diagnosis and treatment protocols, but results of lab testing can have a far-reaching influence because many other downstream decisions are based on lab results. Reflect on this concept and think carefully about where, within your facility, lab results can influence downstream decisions that have the potential to improve patient outcomes or reduce spending.
One of every laboratory’s goals is to make it easier for clinicians to provide the best patient care with cost-efficiency in mind. Laboratories can provide user-friendly test menus and test-order cascade choices. For example, at Tri-Core Reference Laboratories in Albuquerque, NM, providers can order a pregnancy testing care package. If results are negative, no further testing is performed; if they are positive, the lab takes the initiative to notify the provider when the 27-week Glucose Tolerance Test (GTT) and the 36-week Strep B, and any other necessary testing, are due.3 The Tri-Core lab is involved in risk stratification to identify which patients need more care, and it offers order choices that make it easy for the providers to do what is best for the patients.3
Another area where the laboratory can have a positive impact and use analytics to support this is in point-of-care testing (POCT). For example, in certain care facilities with urgent care services, adding a POCT for D-dimer to screen for deep vein thrombosis or pulmonary embolism has the potential to reduce unnecessary admissions or imaging (which are much more costly than the POCT).
Review your lab menu with a fresh perspective and think about specific tests that, with a faster TAT, can have a far-reaching impact in costs and care. For example, implementation of MALDI TOF technology can increase diagnostic efficiency via faster identification of bacteria which can potentially reduce length of stay (LOS). Dr. Brad Brimhall and his colleagues at the University of Mississippi Medical Center used analytics to justify the value of this methodology. They reviewed codes for sepsis and found 710 patients with a LOS greater than two days. Their cost for an overnight hospital stay for a sepsis patient is $1,471.79. With this data, the team determined that the MALDI TOF analyzer would be paid for in only 12.6 weeks—an 80.79 percent rate of return on this project.
The lesson here is to think outside of the cost-center box. A certain methodology may appear expensive on the typical lab cost spreadsheet, but the downstream savings can be more than enough to cover the testing costs and provide a better test methodology that creates revenue for the organization.4
Getting results faster, particularly in certain scenarios, can not only improve patient satisfaction but can potentially eliminate an unnecessary hospital admission or an unnecessary CT scan, or reduce hospital LOS. The average cost of a night in the hospital is approximately $2,000,5 so if a lab can report a result faster, and this allows a patient to be discharged a day earlier, across multiple patients, that can save a significant amount of money. Potential savings generated by these interventions will more than pay for the costs of the lab tests. Think through the entire patient episode of care and determine where a faster lab TAT can decrease hospital admissions, or decrease LOS. And, on the flip side, consider areas where preventive testing can potentially pinpoint a condition before it becomes a more costly chronic disease.
Combining lab data for greater influence
Take this concept of using data for actionable improvements and think about the potential of not only looking at lab data, but combining lab data with other data sets. This business intelligence approach can unlock unlimited potential. Healthcare organizations are using advanced analytics that combine data sets to gain insights about their patient populations in order to improve patient outcomes and decrease spending.
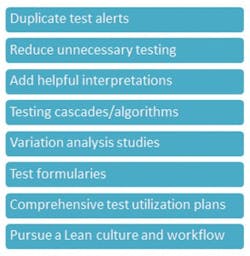
Another example from the University of Mississippi involves a lucrative collaboration between the lab and the pharmacy. Dr. Brimhall partnered with colleagues in pharmacy to improve antibiotic stewardship. Initially it was estimated that as much as $12 million to $15 million per year was being spent on unnecessary pharmaceuticals. The lab and pharmacy performed a study that analyzed the usage of the most expensive antibiotics. Looking at only two antibiotics, they uncovered 2,157 unnecessary doses which equated to a total of $705,877 (variable costs) spent on unnecessary antibiotics. Had those patients been switched to vancomycin this would have cost $56,211, but even subtracting the cost of the vancomycin, this project still resulted in a $649,665 savings (Figure 3).4
Renew your lab strategy
The lab can offer sophisticated diagnostic tools through algorithms, advanced molecular testing, guidance on test utilization, and contributions to analytics that can guide the provider in daily patient interactions and make a substantial contribution to overall organization-wide savings and patient care coordination (Figure 4). By leveraging lab data and combining that data with data from other IT systems, valuable analytic insights can be uncovered. Analytics will drive the future of patient-centered healthcare, and laboratorians are the stewards of a vast amount of the clinical data used to drive treatment plans. Make sure you are making the most of your analytic opportunities.
References
- Centers for Medicare and Medicaid Services. Quality measures and performance standards. CMS.gov. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Quality_Measures_Standards.html. 2015. Accessed December 22, 2015.
- National Committee for Quality Assurance. HEDIS measures. NCQA.org. http://www.ncqa.org/HEDISQualityMeasurement/HEDISMeasures.aspx.
Accessed December 22, 2015. - O’Reilly, K.B. Analyze this: data shines within and without. CAP Today. 2015, November.
http://www.captodayonline.com/analyze-data-shines-within-without/. Accessed December 22, 2015. - Futrell, K. Meaningful medical analytics: Driven by laboratory data integration. June, 2015. http://www.orchardsoft.com/orchard-white-paper-meaningful-medical-analytics-driven-laboratory-data-integration/. Accessed December 22, 2015.
- The Henry J. Kaiser Family Foundation. Hospital adjusted expenses per inpatient day by ownership. 2013. http://kff.org/other/state-indicator/expenses-per-inpatient-day-by-ownership/#. Accessed December 22, 2015.
About the Author

Kim Futrell, MT (ASCP), MSHI
is the Products Marketing Manager at Orchard Software. Prior to joining Orchard in 2012, Futrell, who has a Master of Science in health informatics, worked as a lab manager for more than 20 years.