CONTINUING EDUCATION
To earn CEUs, see current test at www.mlo-online.com under the CE Tests tab.
LEARNING OBJECTIVES
Upon completion of this article, the reader will be able to:
- identify abnormal liver test-result etiologies;
- identify commonly requested liver-function tests and the markers they involve;
- discuss various serum liver enzymes and discuss mild, moderate, and marked elevations in certain of those;
- discuss the elevation of three analytes that measure biliary excretion;
- discuss the measurement of serum-ammonia levels in testing liver function; and
- identify additional markers of liver-disease
There is the classic story of an individual having a dream (i.e., nightmare) where he imagines his individual organs are having a debate as to which is the most important. The heart states, “Without me, blood would stop pumping, and you would die.” The brain states, “Without me, all conscious and autonomic processes would stop.” The lungs state, “Without oxygen, everything else is moot,” and so on. Note: The liver does not get into this debate. It should.
The liver provides a “middleware” solution for many physiologic processes without having a unique organ-specific function as do the heart, lungs, or kidneys. Middleware is software that mediates between an applications program and a network. The liver is middleware since it provides interconnectivity between critical metabolic functions such as processing of the digestion end products, protein synthesis, toxin elimination/breakdown, and excretion of “tough-to-remove” waste products into the bile. It is the poster child for homeostatic processes by maintaining this balance. Illustrative of the liver’s importance is the fact that functional liver failure does not occur until 80% of the liver’s capacity has been damaged beyond repair.1
A relatively small number of common laboratory markers of liver disease exist as well as an even smaller number of uncommonly used disease markers. Most of the markers are either indicative of hepatocyte integrity, biliary excretory ability, or synthetic function.
Anatomy/physiology
The liver is an approximately 1.5 kilograms, solid, irregularly shaped organ composed of four geographic lobes (right, left, quadrate, and caudate) located in the right upper quadrant of the abdomen. It has a dual blood supply consisting of both the hepatic artery (20%) and the portal vein (80%). Both travel the liver via a common entry point and route (portal tract) alongside the bile duct. Portal vein, hepatic artery, and bile duct divide into right and left branches that continually divide and ramify into approximately 450,000 terminal branches.1 Portal-vein supply of blood is unique in that most venous routes directly head toward the lungs for re-oxygenation and are nutrient depleted, whereas the portal vein is nutrient replete and goes through the liver as part of its return trip from the gut. At the outflow end of the liver is the hepatic vein that collects blood from its respective intra-hepatic branches after it passes through the liver. The hepatic vein empties into the inferior vena cava for re-oxygenation and re-circulation. Bile is produced at the level of the hepatocyte, followed by collection into the bile duct for eventual storage in the gallbladder and for use in digestion.
Liver-function tests are not direct measures of liver function
but, rather, indirect measures of liver integrity or biliary-excretory ability.
Hepatocytes are the primary liver cell. They contain high concentrations of mitochondria — large protein-synthesis organelles (endoplasmic reticulum) as well as numerous vacuoles filled with glycogen and lipid. The predominance of mitochondria and endoplasmic reticulum underscore liver functions such as protein synthesis as well as uptake and discharge of numerous components (modified and unmodified nutrients; waste products; and newly synthesized proteins). Hepatocytes are organized into “cords” and “plates” in a multilobular arrangement (each lobule approximately 1 millimeter to 2 millimeters in diameter) with tens of thousands of lobules per liver.
The portal tract and the hepatic vein roughly demarcate the lobule, with branches of the portal tract located at its periphery and the hepatic vein at its center. The lobule is composed of multiple smaller units (acini) and is artificially defined into three zones, with Zone 1 (periportal) closest to the portal tract and Zone 3 (centrilobular) closest to the hepatic vein. Organization of the hepatic parenchyma into lobules and acini between portal tract and hepatic vein allows for a gradual filtration of blood as it moves via sinusoid from Zone 1 to Zone 3. Interwoven throughout the cords are open spaces (vascular sinusoids) that bathe the cells in blood (from both hepatic artery and portal vein), facilitating easy exchange between hepatocyte and blood. As a result, hepatocytes are probably the most perfused cells in the body — explaining why traumatic liver injuries bleed profusely. Contrary to blood flow, bile movement occurs from Zone 3 to Zone 1 via a separate route (bile caniculi to canals of Hering to bile ductules to portal bile ducts.
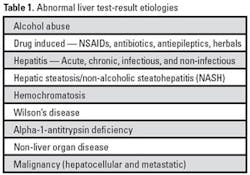
While there are specific markers for specific liver diseases, laboratory diagnosis of such entities usually starts with an abnormal result of a more non-specific test. Liver-related common diseases associated with abnormalities of liver test results are listed in Table 1.2
Regardless of etiology, liver-function tests are not usually tests of function but, rather, tests of hepatocyte integrity or biliary excretory ability. Ironically, tests of synthetic function are not usually ordered to assess liver function but, instead, for another purpose.
Hepatocyte integrity
In the clinical setting, liver-function testing usually refers to serum liver-enzyme measurements and not tests of actual liver function. Serum-enzyme elevation may indicate hepatocyte injury, which can reflect liver-function impairment. The two most commonly requested “liver-function tests” are alanine aminotransferase or ALT (also called serum glutamic pyruvic transaminase or SGPT, and alanine aminotransferase or ALAT. Aspartate aminotransferase or AST (also called serum glutamic-oxaloacetic transaminase or SGOT, and aspartate aminotransferase [ASAT/AAT]). These enzymes are not unique to the liver in either location or function. Respectively, they catalyze the transfer of alpha-amino groups of alanine (ALT) and aspartate (AST) to the alpha-keto group of 2-oxoglutarate to form, respectively, pyruvate and oxaloacetate, in addition to glutamate.3 The enzymes require pyridoxal-5′-phosphate (P5P) as a coenzyme, which is a metabolite of vitamin B6. As a result, as will be discussed, individuals with vitamin-B6 deficiency can have lower-than-expected assayed levels of aminotransferase with resulting clinical and laboratory implications.
Any perturbation to the liver, whether necrosis or not, can induce enzyme leakage from the hepatocyte.
There are multiple assay methods for serum determination of AST and ALT levels. A popular method utilizes coupling of the respective reactions with dehydrogenase reactions: (AST) oxaloacetate —- malate dehydrogenase —-Illustrative of the liver’s importance is the fact that functional liver failure does not occur until 80% of the liver’s capacity has been damaged beyond repair.
ALT and AST are ubiquitous throughout the body but vary in concentration from tissue to tissue. ALT is notable for having a significantly greater concentration in the liver relative to other organs by several orders of magnitude. In comparison, AST is more equally distributed throughout the following organs in decreasing order of concentration: cardiac muscle, skeletal muscle, kidneys, pancreas, lungs, and erythrocytes. Of note, this is one of the pitfalls of elevated AST interpretation as it might reflect, for example, myocardial infarction, rhabdomyolysis, or hemolysis. In fact, AST was historically used as a cardiac marker. AST and ALT are cytosolic enzymes; however, AST also has a mitochondrial component with a much higher concentration than found in the cytosol. ALT has a serum half-life of 40 to 48 hours, and AST has a serum half-life of 16 to 18 hours.
Any perturbation to the liver, whether necrosis or not, can induce enzyme leakage from the hepatocyte. In most situations, degree of serum elevation does not correlate to the type or severity of liver injury but can provide clues. In addition, any elevation of enzymes can occur without apparent clinical finding or symptomaticity.2 Degree of elevation has been divided up into mild (two to three times upper limit of normal); moderate (two to three to 20 times upper limit of normal) and marked (>20 times upper limit of normal).4
Mild to moderate elevations are non-specific and can be due to either liver disease or response to hepatic insult, whether it is acute, chronic, or transient. For example, a night out at the bar can cause a transient elevation in liver enzymes. Mild elevations can be the leading edge of worsening liver disease, muscle injury, viral hepatitis, or congestive liver secondary congestive heart failure. Non-alcoholic fatty liver disease (or NAFLD) (non-alcoholic steatohepatitis [or NASH]) is the most common explanation for asymptomatic mildly elevated liver enzymes in the United States.2
Marked elevations in liver enzymes are a clear indication of severe liver injury such as acute viral hepatitis, ischemic liver injury, and toxin-induced hepatitis. Injury such as acetaminophen toxicity can result in ALT levels ranging in the thousands of U/Ls.5 One important caveat to this discussion is that in severe end-stage liver disease, it is possible for serum enzymes to have normal levels. This reflects a “burned-out” situation where the liver is essentially dead, with minimal viable tissue and minimal enzyme left to leak out.6 A pattern of laboratory results with normal AST and ALT, yet abnormal markers of protein synthesis (prolonged coagulation time, low albumin, or prealbumin levels), is consistent with this clinical situation.7
Examination of the ratio of AST to ALT is also used to help provide clues to the etiology of the liver disease. Normally, the AST/ALT ratio ranges from 0.8 to 1.0; and, in the majority of cases of hepatic injury, this ratio remains the same or decreases. In cases of alcoholic liver disease, however, the ratio is expected to be 2.0 or greater. The probability of alcoholic hepatitis is directly related to the magnitude of the ratio. One study noted that AST/ALT greater than 3.0 was 96% sensitive for diagnosing alcoholic hepatitis.2 An AST/ALT ratio greater than 2.0 occurs in response to two different mechanisms: 1) alcohol-induced expression of mitochondrial AST (three times greater concentration than cytosol) on the surface of the hepatocyte, and 2) alcoholics tend to be malnourished and lacking vitamin B6. As a result, an essential cofactor (P5P) for the assay is lacking, leading to a decreased level of ALT (ALT appears to be more sensitive to a P5P deficiency than AST). In cases of alcoholic liver disease, AST should not go higher than 500 U/L, and ALT should not get past 300 U/L.8
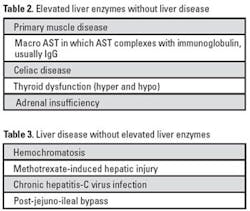
Discordant AST or ALT results to liver disease are possible. Table 2 lists situations where liver enzymes can be elevated without liver disease. On the other hand, Table 3 lists situations where liver disease does not necessarily result in an elevation of liver enzymes.7
Other liver enzymes are lactate dehydrogenase (LD), gamma glutamyl transpeptidase (GGT), and alkaline phosphatase (AP). Use of LD has faded due to its non-specificity and wide distribution in multiple tissue types and organs. GGT and AP will be discussed in terms of biliary excretion.
Biliary-excretory function
Measures of biliary excretion are bilirubin, AP, and GGT. Elevation of all three of these analytes can indicate a biliary-obstructive process, but their respective specificity for obstruction varies. Bilirubin elevations are the least specific, whereas AP elevations are relatively the most specific. Bilirubin metabolism involves transport of the unconjugated insoluble form (bound to albumin) to the hepatocyte where conjugation occurs, increasing its solubility. Conjugated bilirubin is then secreted into the intestine as one of the constituents of bile. In the intestine, the bilirubin undergoes breakdown with 80% excreted and the remainder reabsorbed by the liver.
Bilirubin circulates in serum in the following three forms: 1) unconjugated — bound to albumin, insoluble, and referred to as the indirect fraction; 2) conjugated — soluble and referred to as the direct fraction; and 3) delta bilirubin. This fraction is conjugated but is distinguished by being covalently bonded to albumin. Delta bilirubin shares the same half-life of albumin (20 days), so it remains in serum significantly longer than bilirubin itself (four hours). This provides an explanation as to why elevated serum-bilirubin levels persist in patients with obstructive or intrahepatic jaundice after the obstruction or hepatitis has resolved.9
Many disorders of hyperbilirubinemia (direct and indirect) are due to non-liver-related intrinsic or extrinsic bilirubin disorders of either overproduction (such as hemolysis) or underexcretion. Underexcretion disorders refers to intrinsic enzyme defects in bilirubin metabolism that can lead to elevations in either conjugated (Dubin-Johnson and Rotor syndromes) or unconjugated (Crigler-Najjar and Gilbert syndromes) bilirubin. Liver-associated hyperbilirubinemia occurs in situations where some aspect of the biliary tree is blocked due to either mechanical obstruction (cholelithiasis) or inflammation (cholangitis or primary biliary cirrhosis).
Laboratories commonly report bilirubin as total, direct, and indirect fractions. Normal adult reference ranges are as follows: total bilirubin, 0.2 mg/dL to 1.0 mg/dL, and direct bilirubin, 0.0 mg/dL to 0.4 mg/dL. It is measured using the Jendrassik-Grof reaction, which is a modification of the classic Van den Berghe method. Either method involves addition of a diazo compound to serum, which forms an initial azo compound measured at 540 nanometers, followed by addition of “accelerants” (caffeine or alcohol) to speed up production of the final product at the same wavelength. The initial product is referred to as the direct (soluble, conjugated) fraction, whereas the final product is a measurement of the total bilirubin. The indirect fraction (insoluble, unconjugated) is determined by subtraction of direct from total fractions.9
Alkaline phosphatase is an enzyme of little function that is located throughout the body primarily in liver, bone, intestine, and placenta. It has multiple isoenzymes that can be separated by electrophoresis, if necessary, to determine its source. In the liver, it is located on the canicular surface of the hepatocyte. Obstructive processes will induce AP synthesis and release into the serum. Elevations of AP suggest liver or bone disease. To determine the source, testing for another liver enzyme, GGT, comes into play. If the GGT level comes back normal, then testing for the isoenzymes of AP can be done to determine which is the affected organ.
Gamma glutamyl transferase is located in the following organs in decreasing order of concentration: proximal renal tubule, liver, pancreas, and intestine. The majority of GGT in serum originates from the hepatobiliary system. GGT by itself is a sensitive but non-specific indicator of liver disease. It has been used as a marker of alcohol abuse; and elevations can be seen in a variety of liver conditions, especially those with hepatobiliary involvement. Its primary use is to distinguish elevated AP from either bone or liver sources. If GGT is elevated along with an elevated AP, it is consistent with bilary disease.
GGT is assayed by measurement of a chromogenic end product when GGT catalyzes gamma-glutamyl-p-nitroanilide to liberate p-nitroaniline.
Hepatocyte synthetic function
The liver is the main site of serum protein (albumin) synthesis as well as most of the clotting factors (I, II, V, VII, IX, X, IXX, and XIII). Prothrombin time (PT) is measure of coagulation that utilizes Factor VII as well as Factors I, II, V, and X. As liver function fails, levels of the coagulation factors will drop, and the PT will increase. Improvements in the PT indicate a transient loss of hepatic function, whereas continued prolonged PT is consistent with more significant liver failure. Albumin levels can also be used to monitor liver function; however, its 20-day half-life prohibits its use as a timely measure of liver function. As discussed earlier, normal AST/ALT values with a prolonged prothrombin time (refractory to treatment) is consistent with a poor prognosis.
Serum-ammonia level is another measure of liver function. Ammonia is an amino-acid breakdown product by multiple enzymatic processes that occur in the gut. Ammonia is shunted directly to the liver via the portal circulation where most is metabolized to urea at the hepatocyte Krebs-Hanseleit urea cycle.1 As a result, serum-ammonia levels will be normally very low. Elevated ammonia levels can occur from inherited or acquired disorders. Inherited disorders manifest during infancy and have no cure; however, special diet and medications can minimize the disorder’s impact. Acquired disorders occur in advanced liver and renal diseases. Associated with hyperammonemia is a condition known as hepatic encephalopathy. Ammonia is measured using alpha ketoglutarate catalyzed by glutamate dehydrogenase to yield glutamate with the oxidation of NADPH to NADP. The decrease in NADPH is monitored by decrease in absorbance at 340 nanometers. Measurement of serum ammonia is very subject to preanalytic interferences that include room-temperature storage and cigarette smoke. Additional markers of liver disease are listed in Table 4.8
In conclusion, liver-function tests are not direct measures of liver function but, rather, indirect measures of liver integrity. When ordered, the most often requested tests are for AST and ALT. Elevations of either can indicate possible liver disease. The possibility of liver disease based on those markers depends on magnitude of increase as well as ratio of AST to ALT. Another indirect measure of liver function is markers of biliary excretion (bilirubin, GGT, and AP). Elevation of any of these has the possibility of diagnosing some obstructive impairment to biliary excretion. Last, the liver is the site of synthesis of both albumin and clotting factors. As a result, decrease in albumin concentration or prolongation of prothrombin time can be consistent with derangement of liver function. There are numerous algorithms available in the literature with which readers can follow up to review common sequences of testing that clinicians use to evaluate abnormal results.10,11,12 Most perturbations of liver function can manifest as abnormal liver-test results before clinical findings are apparent. Abnormal test results should be followed up by alternative testing and clinical examination of the patient.
David Alter, MD, is a clinical/chemical pathologist in Pathology and Laboratory Medicine at Spectrum Health-Blodgett in Grand Rapids, MI.
References
- Crawford JM. Liver and Biliary Tract. In: Kumar V, Abbas A, Fausto N, eds. Robbins Pathologic Basis of Disease. 7th ed. Philadelphia, PA: Elsevier/Saunders; 2006:877-937.
- Pratt DS, Kaplan MM. Evaluation of abnormal liver enzyme results in asymptomatic patients. NEJM. 2000:(342);1266-1271.
- Panteghini M, Bais R, Van S. Enzymes. In: Burtis CA, Ashwood ER, Bruns DE, eds. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. 4th ed. St. Louis, MO: Elsevier/Saunders;2006:597-644.
- Ahmed A, Keefe, E. Liver Chemistry and Function Tests. In: Feldman M, Friedman L, Brandt L, eds. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease 2006: www.accessmedicine.com. Accessed November 10, 2008.
- Johnston DE. Special consideration in interpreting liver function tests. AAFP. 1999;59:2223-2230.
- Pincus M, Tierno PM, Dufour DR. Evaluation of Liver Function. In: McPherson RA, Pincus MR, eds. Henry’s Clinical Diagnosis and Management by Laboratory Methods. 21st ed. St. Louis, MO: Elsevier/Saunders;2007:263-278.
- Chopra S. Patterns of plasma aspartate and alanine aminotransferase levels with its liver disease. In: Basow DS, ed. UpToDate. Waltham, MA; 2008. www.uptodate.com. Accessed October 23, 2008.
- Dufour DR. Liver Disease. In: Burtis CA, Ashwood ER, Bruns DE, eds. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. 4th ed. St. Louis, MO: Elsevier/Saunders; 2006;1777-1848.
- Higgins F, Beutler E, Doumas BT. Hemoglobin, Iron and Bilirubin. In: Burtis CA, Ashwood ER, Bruns DE, eds. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. 4th ed. St. Louis, MO: Elsevier/Saunders; 2006;1165-1208.
- American Gastroenterological Association. Evaluation of Liver Chemistry Tests. Gastroenterology. 2002;123:1364-1366.
- Pratt DS, Kaplan MM. Evaluation of Liver Function. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J, eds. Harrison’s Principles of Internal Medicine. 2008. www.accessmedicine.com. Accessed November 17, 2008.
- Dufour DR. ed. Laboratory Guidelines for Screening, Diagnosis and Monitoring of Hepatic Injury. National Academy of Clinical Biochemistry, 2000.
MLO’s Continuing Education Test is available online only.
Print out and mail a copy with your check, or use the new online CE test and convenient online payment feature available through the auspices of Northern Illinois University.
Go to www.mlo-online.com and look under CE Tests.