A holistic approach to error prevention in the clinical laboratory
In the world of clinical laboratory testing, precision and accuracy are paramount because laboratory results can have a critical impact on patient safety, so preventing errors is non-negotiable. Yet, the challenge for laboratory leaders lies not only in the sophistication of the tests performed, or the selection of appropriate tests, but also in the intricacies between technology, systems, and human capital. To address this complex challenge, a comprehensive strategy that encompasses structural, technological, and cultural measures is essential. From meticulous policies and procedures, or advanced hardware and relevant software, to fostering a culture of open communication, psychological safety, and continuous improvement, the integration of these elements creates a holistic defense against the errors in the clinical laboratory, ensuring the reliability and integrity of test results.
Errors in the total testing process
The total testing process (TTP) involves multiple steps to ensure accurate and reliable results. This journey comprises pre-analytical, analytical, and post-analytical phases and demands meticulous attention to detail at every turn. It begins with healthcare providers ordering specific tests, followed by the collection and proper labeling of patient specimens. After transportation to the laboratory, specimens undergo processing, and tests are performed. The generated data is analyzed, and results are reported to healthcare providers for interpretation in the context of patient information. Diagnostic decisions are made based on the results, and the data is archived for reference and quality assurance.
In the pre-analytical phase, errors emerge from specimen handling, utilization, ordering, transportation, collection, and patient identification. A misstep at any of these preliminary stages can cast a long shadow, influencing the reliability of subsequent test results. Analytical errors, on the other hand, may arise from a variety of sources, including reagent issues, calibration discrepancies, quality control, and instrumental malfunctions. These errors have the potential to skew results, introducing inaccuracies that, if undetected, could lead to misguided clinical decisions.
The post-analytical phase, often regarded as the final frontier before results reach the clinician's hands, is not exempt from its share of challenges. Data entry and management errors, miscalculations, and reporting inaccuracies pose threats to the integrity of the diagnostic process. Whether it be calling critical values erroneously or overlooking essential delta checks, the post-analytical realm demands an extra layer of scrutiny. Moreover, measurement conversion errors and misinterpretations further underscore the fragility of this intricate process.
As laboratories strive for excellence, understanding and mitigating errors across the entire total testing process becomes imperative—where the journey from specimen to result is not merely a sequence of steps, but a delicate orchestration of precision and diligence.
Three pillars of prevention
To prevent errors effectively, laboratory leaders must adopt a proactive stance, implementing rigorous measures and fostering a culture that places a premium on error reduction through three pillars: structural prevention, technological prevention, and cultural prevention. In this intricate management of science and diligence, the pursuit of error prevention in the clinical laboratory emerges not merely as a task, but as a solemn commitment to the well-being and trust of the patients relying on the precision of diagnostic outcomes.
Structural prevention establishes the foundation for a robust defense against errors. Detailed policies and procedures, spanning testing protocols, quality control measures, and standardized operating procedures, provide a structured framework that guides laboratory operations. Regular assessments of the laboratory's Quality Assurance/Quality Management (QA/QM) plan ensure that these structures remain dynamic, adaptive, and aligned with the evolving landscape of healthcare. Structural prevention sets the stage for systematic checks and balances, creating an environment where errors are less likely to occur due to procedural lapses or ambiguities.
Technological prevention introduces a layer of sophistication, leveraging hardware, software, and information systems to fortify the laboratory's defenses. Advanced hardware, such as positive patient identification systems and barcoding solutions, enhances accuracy in specimen handling and processing. Automated temperature monitoring and quality control applications bring precision to critical aspects of testing, reducing the likelihood of errors stemming from environmental or procedural fluctuations. Laboratory information systems (LIS) play a crucial role, ensuring correct builds and seamless integration of testing platforms, diminishing the risk of errors associated with data transfer and interpretation.
Cultural prevention, the third pillar, represents the human aspect of a holistic defense against errors. Cultivating a culture of laboratory safety and continuous improvement establishes a philosophy where every team member actively contributes to error prevention and where the laboratory leadership fosters psychological safety. Effective feedback mechanisms, coupled with routine competency checks and ongoing training, create a dynamic learning environment where errors are not only addressed but serve as catalysts for improvement, as opposed to punishment.
Putting it all together
Laboratorians are entrusted with the responsibility of ensuring the integrity and precision of the diagnostic process, making the implementation of the three pillars of prevention—structural, technological, and cultural—a crucial endeavor.
To fortify the structural foundation, leaders should invest in developing and regularly updating comprehensive policies and procedures. These documents should serve as living guides, reflecting the latest industry standards, and continuously evolving to address emerging challenges. At the same time, a proactive approach involves routinely assessing the Quality Assurance/Quality Management (QA/QM) plan, ensuring that it aligns with the laboratory's goals and regulatory requirements. Laboratory leaders need to be intimately familiar with the laboratory’s QA/QM plan and regularly assess it for improvement. This continual scrutiny ensures that structural preventive measures remain robust, adaptive, and relevant.
Technological advancements offer a powerful arsenal in the fight against errors. Laboratory leaders should prioritize investments in cutting-edge hardware and software solutions. Positive patient identification systems, barcoding technology, and advanced communication systems bolster accuracy in specimen handling and result reporting. Automated temperature and humidity monitoring applications, quality control interfaces, and cybersecurity measures also contribute to the integrity of laboratory processes. Additionally, a focus on optimizing the laboratory information systems (LIS) ensures correct builds and seamless integration with testing platforms, which can further minimize the risk of errors related to data interpretation.
Cultural prevention, the often undervalued yet highly effective pillar, demands intentional leadership. Laboratory leaders should foster a culture that places all forms of safety at the forefront and embraces continuous improvement as a collective mission. Establishing open communication channels encourages team members to voice concerns and report errors without fear of retribution. Creating effective feedback systems, along with routine competency assessments beyond what CLIA requires, instills a mindset of perpetual learning and growth. Laboratory leaders must champion the concept of total quality management, making quality assurance a shared responsibility among all team members. By embedding these cultural values into the fabric of daily operations, leaders inspire a collective commitment to laboratory excellence and patient safety.
Final remarks
The synergy of these three pillars is vital to effective error mitigation. The structural, technological, and cultural elements are interdependent, each reinforcing the others to create a resilient defense against the complexities of the total testing process. It is important to note that if one is neglected, the remaining two pillars can only be partially effective.
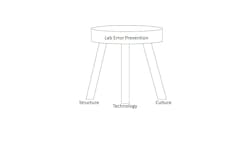
Like a three-legged stool (Figure 1), each pillar plays a crucial role, contributing to the stability and effectiveness of the overall preventive framework. If one pillar fails, the consequences can resonate throughout the entire laboratory system. A deficiency in structural measures may lead to procedural ambiguities and lapses, compromising the reliability of testing processes. Technological shortcomings could introduce inaccuracies, jeopardizing the interpretation of results and the security of data. A lapse in the cultural pillar will result in communication breakdowns, diminished vigilance, and a declining sense of collective responsibility for quality assurance. The interconnection of these pillars underscores the importance of maintaining equilibrium; any imbalance has the potential to weaken the laboratory's ability to safeguard against errors, which ultimately impacts patient care.
Embracing these pillars requires a strategic, forward-thinking approach—one that recognizes errors as multifaceted challenges and addresses them comprehensively. As leaders commit to the implementation of these preventive measures, they not only safeguard the integrity of laboratory results, but also foster a culture of excellence, innovation, and unwavering dedication to providing the highest standards of patient care.
About the Author

Stephen Bishop, MBA, MS, CLS, MLS(ASCP)CM, CPHQ
MBA, MS, CLS, MLS(ASCP)CM, CPHQ
is currently the Market Director of Laboratory Services at CommonSpirit Health, Southern California. Stephen is passionate about healthcare leadership, clinical laboratory education, and process improvement.