What makes lab innovators worth watching? They develop procedures or processes to improve testing, allowing for faster and more accurate diagnoses, treatments and, ultimately, better patient outcomes.
In Medical Laboratory Observer’s (MLO) inaugural Lab Innovators Worth Watching, we profile organizations that are making a lasting impact on patients’ health and well-being.
Kaiser Permanente in California begins
COVID-19 testing
Its reference laboratories associated with the Permanente Medical Groups are no exception. Divided into southern and northern regions, the California labs have responded to COVID-19 by bringing testing in-house, allowing the healthcare giant to expand testing capacity for anxious patients.
In fact, just one week after Roche Diagnostics received an emergency use authorization (EUA) from the Food and Drug Administration (FDA) for its cobas SARS-CoV-2 Test, the labs began analyzing specimens using the assay. The test is performed on Roche’s cobas 6800 instrument in Southern California and the cobas 8800 instrument in Northern California.
Patients and their providers generally receive results in between 18 and 24 hours, which includes the time it takes to transport the specimens from medical clinics to the labs.
The Southern California regional reference labs, which include facilities in Chino Hills and North Hollywood, began processing about 750 tests daily, which has quickly increased to approximately 1,600 tests daily. The Northern California reference lab is in Berkeley.
The workflow for the test is integrated into the electronic health records (EHR) and laboratory information system (LIS), allowing orders and results to flow back and forth electronically. Positive test results also are called into the medical center that ordered the test or a Kaiser Permanente COVID-19 command center.
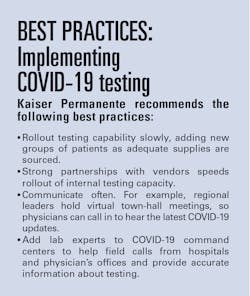
Rolling out the test so quickly required that the reference labs work with the region’s infectious disease physicians, information technology department and EMR support and regional COVID-19 command centers.
In addition to the challenges of coordinating among numerous groups to develop processes and workflows, the regional labs in Southern California also had to validate the test against several swab types and transport media, including sterile saline. Even so, Kaiser Permanente is still struggling to purchase enough swabs for the tests.
In Southern California, the tests are currently offered to healthcare workers, first responders and symptomatic patients in hospitals, emergency departments, long-term care and skilled nursing facilities and medical clinics.
In addition, “having the test with a more rapid turnaround time (TAT) and capacity to perform testing allowed the group to open up testing to patients in outside affiliated hospitals as well as to hospitals outside of the Kaiser Permanente system, who were in desperate need of more rapid testing results,” said Timothy M. McSkane, Executive Leader for the Laboratory Care Delivery System for the Southern California Permanente Medical Group, in a nomination letter to MLO.
McSkane and Steven R. McLaren, DO, Assistant Regional Medical Director at the Laboratory Care Delivery System, nominated eight individuals for their work in rolling out COVID-19 testing in California.
At the Southern California Permanente Medical Group Regional Reference Laboratory, those people are: Jonathan Gullett, MD, Physician Director in Microbiology; Kenneth Van Horn, PhD, Technical Director in Microbiology; Vahe Khanlian, CLS, Director of Operations for Microbiology Services in North Hollywood; Onie Bueno, CLS, Director of Operations for Microbiology Services in Chino Hills; Nimfa Burgos, CLS, Assistant Operations Director in Immunology in North Hollywood; Sienna Mendoza, CLS, Assistant Operations Director, Bacteriology and Molecular Infectious Disease; and Robert Elazegui, MHA, CLS, MLS, Operations Manager in Molecular Infectious Disease in Chino Hills.
At The Permanente Medical Group in Northern California, McSkane and McLaren nominated Jeffrey Schapiro, MD, Associate Medical Director of the Regional Reference Laboratory and Brian Missett, MD, Associate Executive Director of the medical group.
The northern and southern regions are not standing still. Both regions are considering adding two additional tests: Abbott’s Real time SARS-CoV-2 rRT-PCR and Cepheid, Xpert Xpress SARS-CoV-2.Kaiser Permanente molecular genetic pathology lab adopts non-invasive test
Kaiser Permanente’s Southern California Molecular Genetic Pathology Regional Reference Laboratory improved the lives of pregnant women substantially when it brought a non-invasive prenatal test in house that is based on analyzing Cell Free DNA (cfDNA) in blood samples.
Bringing testing capability in-house reduced the turnaround time from seven to 10 days to two to three days and saves Kaiser Permanente’s Southern California region $1 million annually in external lab costs.
The test is used to screen fetuses for Down syndrome, Edwards syndrome (Trisomy 18) and Patau syndrome (Trisomy 13). It also can determine fetal sex. The test, which can be performed as early as 10 weeks gestation, is generally safer than chorionic villus sampling (CVS) or amniocentesis, which both carry a slight risk for miscarriage.
The molecular genetic pathology lab conducts the tests using next-generation sequencing (NGS) on the Illumina platform. Normal test results are routed to patients through the KP.org patient portal while abnormal results are sent to genetic counselors.
The program has been so successful that Kaiser Permanente is evaluating whether to expand it to other regions in the organization.
McSkane and McLaren also sent a nomination letter to MLO’s Lab Innovators Worth Watching for this project, naming Ruan Ramjit MD, Physician Director; Mike Moradian, PhD, Director of Operations; and Anatole Ghazalpour, PhD, Technical Director.The Center for Telehealth at the University of Mississippi Medical Center reduces HbA1c
Sometimes a lab innovator isn’t a medical scientist, technician or pathologist. That’s the case with Tearsanee Davis, DNP, FNP-BC, who is the Director of Clinical and Advanced Practice Operations for the Center for Telehealth at the University of Mississippi Medical Center in Jackson, MS.As director, she leads the Center for Telehealth in its work to address chronic diseases—particularly among rural low-income populations. When patients enroll in the telehealth program, the staff then teaches patients about self-testing and self-care at home, using Bluetooth-enabled digital monitoring devices, such as glucose monitors and tablets.
Many of these patients find it challenging to make it to in-person appointments both with specialists and with labs for routine testing because of living in underserved areas. But without proper testing, patients could have medical regimens that aren’t optimized for their needs, potentially leading to a deterioration in their chronic illnesses.
To address these problems and improve the health of chronically ill Mississippi residents, the Center for Telehealth began a study in 2014 to evaluate a telehealth-based approach to managing patients with diabetes in Sunflower County—a geographic area with a population of 25,000 and a median income of $30,029.1
The Mississippi Diabetes Telehealth Network was formed to conduct the study, and included the University of Mississippi Medical Center (UMMC) and General Electric (GE), which provided the equipment for education and biometric data collection; North Sunflower Medical Center (NSMC), which provided the rural clinic; and Telepex, based in Jackson, MS, which provided free wireless connections through its C Spire service.2
In addition to at-home monitoring, each patient in the study also attended quarterly appointments at the rural clinic, which included blood tests.
A total of 115 patients completed the 12-month study program. The study logged impressive results, including a significant difference in in HbA1c, total cholesterol, low density lipoproteins (LDL), high density lipoproteins (HDL), triglycerides, creatinine clearance, glomerular filtration rate and potassium.
Jamie Phillips, PhD, Senior Scientific Affairs Manager at Roche Diagnostics, who nominated Davis for Lab Innovators Worth Watching, explains, “Dr. Davis’ work has impacted clinical laboratory operations by promoting better patient care through patient self-testing and the use of telehealth.”
Phillips also notes that nurses involved in the telehealth program can remind patients about their quarterly in-person blood tests, helping ensure that patients keep their appointments. “Dr. Davis is 100 percent a lab innovator by ensuring the lab testing can be completed by the patient to ensure the cadence of testing can occur in rural and low-income areas…pretty innovative!”
References:
- Census.gov. (2019). Quick Facts: Sunflower County, Mississippi. U.S. Census Bureau [online] Available at: https://www.census.gov/quickfacts/sunflowercountymississippi [Accessed 6 April 2020].
- Davis T, Hoover K, Keller S, Replogle W. Mississippi Diabetes Telehealth Network: A collaborative approach to chronic care management. Telemedicine and e-Health. 2020; 26: 185-189.