Introducing point-of-care hematology testing in rural Papua New Guinea
Papua New Guinea is a country of over 8 million people just to the north of Australia. Characterized by its tropical climate, rugged terrain, and a predominantly rural population, most people live in remote areas, making access to healthcare services extremely challenging. Healthcare delivery in this region suffers greatly from a lack of resources, including poor infrastructure and a shortage of healthcare workers. The ratio of doctors to people is 0.5 to 10,000, and nurses only 5 to 10,000. With life expectancy sitting at 65 years, and an excessively high maternal and infant mortality rate, access to care in Papua New Guinea is in dire need of innovation.
St. Mary’s Hospital is located in Vunapope, Kokopo, the capital of East New Britain, an island to the north of the mainland of Papua New Guinea with a population of approximately 400,000. The range of disorders requiring acute care at the hospital generally includes various infections such as community-acquired pneumonia, tuberculosis, and malaria. Diabetes, stroke, myocardial infarction, and other outcomes of cardiovascular diseases are also a significant percentage of admissions.
Challenges
Outdated testing methods
Blood films are made at the time of collection and stained for examination by the laboratory scientists trained in blood cell morphology. A desktop biochemistry machine performs a range of biochemistry tests, including electrolytes, urea, creatinine, and liver function tests using prepackaged kits with specific test sets. A blood transfusion service exists with the capability to do HIV, hepatitis B, or syphilis testing and standard cross-matching for ABO and Rh.
Utilizing these outdated testing methods is time-consuming, resource-heavy, expensive, and prone to operator errors. The processes are complex, with machinery requiring extensive upkeep, regular replacement of reagents, and operation by trained technicians. In addition, these modes of operation often leave patients waiting from hours to days for critical test results, delaying the initiation of treatment.
Inconsistent results
Clinicians at St. Mary’s see regular inconsistencies in their hemoglobin measurements, noting fluctuations in tests performed a day apart from the same patient, with no obvious reason for the variation. These irregularities have affected decisions for transfusions, hindering and delaying effective triaging and treatment of patients in need.
Offering an extra white cell count is important as it is the only laboratory result available as an indicator of infection. However, St. Mary’s currently utilizes the Niebauer technique to collect these results—a time-consuming process that is subject to technical problems. White cell count differentials are necessary to establish a neutrophil count and are generally satisfactory, but staining the blood films can be a problem due to inconsistent staining techniques.
While platelet counts can be assessed manually, in some critical cases, blood samples have been sent to another hospital where they have a desktop hematology analyzer. However, there is no laboratory information system, so results are sent back on handwritten paper. This tedious process can take days while physicians wait to properly diagnose, treat, and triage their patients.
Staff shortages
St. Mary’s Hospital faces a severe lack of resources, employing just 54 nursing officers, 50 community health workers, 1 health extension officer, and 3 doctors. Between 2019 and 2020, there were 4,158 admissions; 2,076 newborn deliveries; and 111,729 visits to the hospital’s outpatient and emergency departments. This challenge puts considerable pressure on St. Mary’s healthcare workers and highlights the need for innovative tools and instruments that can assist them in more effectively managing the limited resources they have.
Solution
It was recognized that a modern hematology analyzer would greatly alleviate the struggles being faced by medical staff at St. Mary’s Hospital. A new hematology analyzer was provided to their laboratory in April 2021—an initiative by the point-of-care testing team from New South Wales Pathology. The aim was to evaluate how the new analyzer would impact the hospital, doctors, and patients in Papua New Guinea.
The analyzer provided point-of-care complete blood counts (CBC), which was a perfect fit for St. Mary’s needs. The portable device delivered lab-quality diagnostic information from a single finger-prick of blood within 5 minutes, allowing healthcare professionals to make treatment decisions in real-time. The device is equipped with viscoelastic focusing (VEF), along with AI-powered machine vision and “lab-on-a-cartridge” technology.
The compact and lightweight analyzer allows for easy installation and utilization in rural settings. Because it is so easy to operate and requires no calibration or maintenance, minimally trained operators can achieve diagnostic accuracy on par with the best hospital laboratories, resulting in lower operating costs and significant enhancements to patient quality of life. This helped to overcome multiple challenges St. Mary’s Hospital faced, including shortage of staff, lack of resources, and the slow time frame in triaging and diagnosing its patients.
Transforming care delivery
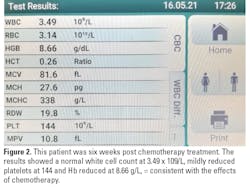
Implementing the device as a point-of-care CBC solution at St. Mary’s Hospital addressed the challenges they faced, particularly timely treatment of its patients. Since April 2021, some of the important diagnoses made included the following:
- Three patients were diagnosed with leukemia.
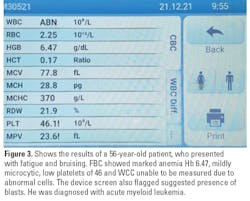
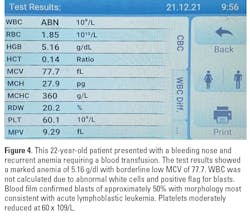
- Two patients were diagnosed with acute leukemia.
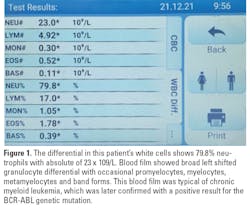
- One patient was diagnosed with chronic myeloid leukemia.
Conclusion
References
- PixCell Medical. PixCell Medical to enhance NSW health pathology’s point-of-care testing service. PR Newswire. Published December 2, 2020. Accessed June 9, 2022. https://www.prnewswire.com/il/news-releases/pixcell-medical-to-enhance-nsw-health-pathology-s-point-of-care-testing-service-836150059.html.
Dr. Yaara Ben-Yosef is a regulatory and clinical affairs expert with a successful track record in the research and development of complex biological processes for the healthcare industry. She also has experience in clinical trials design and monitoring and regulatory affairs management. Yaara holds a BSc (Summa cum laude) in Biology, an MSc in Medical Sciences, and a PhD in Medical Sciences, all from the Technion Israel Institute of Technology.
About the Author

Dr. Yaara Ben-Yosef
is a regulatory and clinical affairs expert with a successful track record in the research and development of complex biological processes for the healthcare industry. She also has experience in clinical trials design and monitoring and regulatory affairs management. Yaara holds a BSc (Summa cum laude) in Biology, an MSc in Medical Sciences, and a PhD in Medical Sciences, all from the Technion Israel Institute of Technology.