Lab managers strive to improve both the quality and efficiency, or value, of their operations.
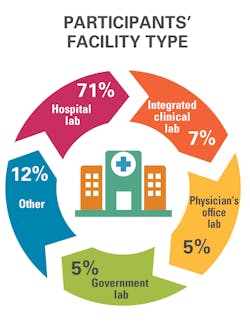
That was the message that came through in Medical Laboratory Observer’s (MLO) second State of the Industry survey, which focused on management best practices. In all, 225 people responded to MLO’s 31-question survey. Most of them (71 percent) work in hospital-based labs, are in management (65 percent), and are at least 56 years old (61 percent).
As one survey respondent—Richard Cole, lab manager at Effingham Health System in Springfield, GA— explained in an interview, “We are so busy in the lab. We are asked to do things faster and quicker with fewer people.”
And as providers, including health systems and hospitals, sign more and more payment contracts based on value-based care, the pressure on labs to ratchet up quality and efficiency will continue.
In a position statement on value-based care published in May 2017, the American Association for Clinical Chemistry (AACC) said, “Laboratory testing is critical to the success of this new model. Clinicians routinely order tests to diagnose their patients, make treatment decisions and monitor therapy, so it is vital that the right tests are ordered and appropriately interpreted. Without this judicious use of the laboratory, patient care suffers and healthcare costs needlessly increase.”Incorporating IT
Thinking about the implications of value-based care, MLO asked survey participants about the strategies they’ve implemented to improve efficiency, ensuring that reimbursement covers their costs. MLO also asked them to rank the effectiveness of each of these strategies on a five-point scale, with five being the most effective. (Respondents only ranked the effectiveness of strategies they’ve adopted in their institutions).
In the most common answer, 60 percent of respondents said they’ve incorporated information technology (IT) to reduce human errors. Most of them thought adopting IT to achieve this goal was effective, with 65 percent rating it with a four or five and 27 percent giving it a three.
Cole is among the respondents who are in favor of adopting IT to reduce human errors. In 2019, Effingham Health System, a critical access provider, purchased software interfaces to transmit test-result data directly from point-of-care (POC) testing devices to its electronic health record (EHR), which also includes the laboratory information system (LIS).
The goal for the hospital was to minimize key-stroke errors, which can occur when harried lab techs enter test results into patients’ records.
In the first phase of the project, the lab focused on tests that generate a positive or negative result, including tests for pregnancy, flu, strep and respiratory syncytial virus, or RSV. In these cases, technologists no longer are involved in reporting test results in the EHR. Because the results are reported as positive or negative, the hospital also turned on auto verification, Cole said.
In the second phase of the project, the health system added interfaces to transmit result data from POC cardiac biomarker tests to the EHR. Since these results are numeric, however, lab techs review critical values manually before the results are recorded in the EHR.
Among all survey respondents, implementing IT to help keep up with ever-changing regulations was less common than solutions to reduce errors. Slightly more than one-third, or 36 percent, said they’ve incorporated IT for this purpose.
Adopting other efficiency-boosting strategies
Nearly as many respondents, or 51 percent, have created standard lab processes and staff education materials. This strategy also received strong ratings for effectiveness: 65 percent assigned it a four or five for effectiveness and 27 percent gave it a three.
Regularly analyzing processes to look for savings opportunities is another way 27 percent of survey respondents ensure that reimbursement covers their costs, while 28 percent have incorporated waste and efficiency studies aimed at reducing overhead.
Given the shortages of qualified lab personnel, labs not only want to standardize their operations but also automate them, which reduces demand for full-time equivalents (FTEs). One way to accomplish that goal is by automating testing processes, and 48 percent of survey respondents said they’ve adopted analyzers that provide walkaway testing to do just that. A total of 65 percent rated this strategy with a four or five for effectiveness and 27 percent gave it a three.Setting Capital Spending Priorities
While implementing IT tools and automation products are important ways for labs to improve efficiency, how do managers decide which projects to fund? In the survey, MLO asked respondents to select their top priority for capital investments. They were nearly evenly divided among three options: 33 percent of them chose technology to remain competitive as their top priority, 32 percent chose technology to cover broken equipment and 27 percent chose automation technology to reduce their FTE requirements. Another 8 percent of them chose the “other” option.
Among those who picked “other,” some explained their choice. Their goals for capital projects included:
- Technology to remain innovative and best meet the needs of our patient population
- Technology that improves turnaround times (TAT), advancing patient care, patient satisfaction and reducing patient stays and wait times
- Cost-effective equipment that improves workflows and patient outcomes.
Implementing new solutions
Choosing a piece of lab automation equipment is just the beginning. Labs also need to install the products. When asked about the best practices they use to get new equipment into daily operations, more than two-thirds (70 percent) said they analyze workflow processes to ensure proper space planning, 49 percent involve the IT department early in the implementation process and 25 percent designate a staff member as project manager.
- Train-the-trainer model (64 percent)
- Standard workflows for all employees (53 percent)
- Mandatory training for all new employees that is led by IT department staff members (25 percent)
- Formal LIS training for one employee, so he or she can become the in-house expert (22 percent)
- Lunch-and-learn sessions (21 percent).
Reining in consumable supply costs
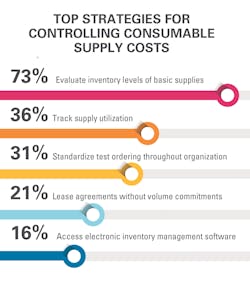
Consumable supplies can be expensive. That’s why a majority (73 percent) of lab employees who participated in the survey said they evaluate inventory levels regularly for basic supplies, such as assays and reagents. And 36 percent have implemented processes to track supply utilization, but only a minority of them (16 percent) have secured access to electronic inventory tracking from their organization’s materials management department.
And a small number (14 percent) have developed ongoing reviews to compare supply reports with the number of invoiced tests.
At 99-bed Labette Health in Parsons, KS, supervisors in each section are responsible for tracking inventory levels, and the process works well for most areas.
The exception is chemistry, where managers use spreadsheets to track consumables, but the process is cumbersome. “It’s a volume issue,” said Janet Cruse, lab manager at Labette Health. The chemistry workload is more prone to spikes from special events, such as health fairs, which makes tracking and projecting supply needs even more challenging, she noted.
To solve the problem, the lab plans to eliminate spreadsheet-based monitoring of consumables by purchasing analyzers capable of automatically tracking inventory.
“One of the deciding factors will be the ability to control inventory in the chemistry area,” she added.Implementing efficient contracts
Streamlining the contracting process is another way to manage costs.
The majority (73 percent) of survey respondents said they are working with their organization’s supply-chain department to increase the amount of supplies they order through group purchasing contracts, which typically offer additional savings. Slightly more than half of them (51 percent) have adopted ongoing reviews of reference lab costs and contracts.
Improving relationships with vendors is another way labs strive to save money. For example, 28 percent of survey respondents signed longer contracts, such as a seven-year agreement instead of a one- or two-year agreements. Slightly more than half (52 percent) have improved their relationships with vendors’ representatives, which helps ensure access to training and product-optimization suggestions.
With consumable supplies specifically, a smaller percentage (21 percent) of survey respondents have signed lease agreements that do not include volume commitments for consumables, while 13 percent have implemented vendor-managed ordering.
Improving testing quality and efficiency
But success in a value-based reimbursement environment, isn’t just about managing costs. Boosting quality also is important. In labs, monitoring room temperatures is a particularly important way to ensure the accuracy of test results. That’s why it is not surprising that more than half of survey respondents, or 54 percent, have evaluated temperature-monitoring equipment and procedures.
While labs have undoubtedly addressed quality improvement through numerous other internal initiatives, MLO also asked survey respondents about the steps they’ve taken to ensure that physicians and other providers order tests correctly.
Here’s what they said:
- 72 percent standardized ordering procedures and formularies
- 24 percent implemented a preapproval program for tests that are send outs
- 27 percent implemented evidence-based test utilization backed by data
Indeed, lab professionals are instrumental not only in improving how providers order and interpret tests, but also in how lab personnel conduct testing and results reporting. Through their efforts, lab professionals boost both the quality and efficiency of patient care, helping to ensure the financial resiliency of their organizations.