Infection prevention is a major focus of the healthcare industry—perhaps more than many laboratory directors realize. In 2014 this market was estimated at $13.1 billion, including chemical and physical equipment solutions. The highest rate of growth is the $3.1 billion sector represented by disinfection and sterilization equipment. This is impacted by increasing biocide regulations that drive a need for alternatives to certain chemical approaches. The infection prevention sector ranges from solutions for small medical devices to wide area/room units and covers both contact and airborne pathogen sources.
Protecting patients from healthcare-acquired infections (HAIs) has rightly received increasing focus in recent years. In general, there has been a bit less emphasis on protecting clinical laboratory scientists from what might be called “laboratory-acquired infections” (LAIs). This is changing, however. In 2014, following a series of LAIs and breaches in safety protocol, the Centers for Disease Control and Prevention (CDC) established the Laboratory Safety Workgroup. This advisory committee has been tasked to review existing practices and identify opportunities to improve laboratory worker safety. Emerging technology trends in HAI prevention can be applied to the laboratory and considered for additional levels of protection there as well.
Controlling surface pathogens
Chemical means of disinfection have been, and will continue to be, a practice in controlling surface pathogens. However, with resistant organisms on the rise, physical processes such as ultraviolet (UV) and gamma irradiation are receiving increasing attention. In UV disinfection, light in the range of 250-280 nm disrupts the DNA of microorganisms, rendering them unable to reproduce. The action spectrum for bacteria is commonly reported as 265-267 nm peak wavelength, although wavelength susceptibility may vary among the large number of bacterial and viral strains. Using UV irradiation with the proper dosage and wavelength on lab surfaces may allow laboratorians to disinfect their workspace without having to worry about germ resistance or needing to use increasingly harsh chemicals.
In 2008, portable wide-area units were introduced into the market to disinfect hospital patient rooms in between stays and decrease HAIs. These early units were able to fully disinfect a patient room in approximately six hours. Innovations and improvements allow today's units to achieve disinfection times of a few minutes. Hundreds to thousands of hospitals now systematically use this surface decontamination technique and have documented improved health outcomes of greater than 50%.
Adoption of this method in laboratory environments has been slow to date, due in part to design limitations and the expense posed by existing lamps. As the performance of LEDs that emit germicidal wavelengths (UVC LEDs) improves, they are becoming a suitable light source option for these applications. The small footprint of UVC LEDS allows them to be placed in a variety of spaces and configurations, or integrated into battery-operated units that can disinfect surfaces on demand. Additionally, the wavelength of LEDs is tunable, meaning they can be tailored to a specific wavelength to target the action spectra of a particular bacterial or viral strain.
Disinfection for airborne diseases
The primary source for LAI occurs through inhalation. Many procedures mitigate this risk through use of personal protective equipment (PPE) and other physical barriers. However, integration of upper room germicidal irradiation (UVGI) could provide another level of protection for workers. This method of disinfection has been found to reduce rates of infection by 80% in controlled mammalian laboratory experiments published by Ed Nardell, PhD, Harvard Medical School.
arrangements using UVC LEDs
Traditional upper room UVGI systems use mercury lamps as UVC light sources and are left on continuously in occupied rooms and congregate settings. Careful safety precautions, such as directing almost all of the UV light above eye-level, are important design considerations. With traditional mercury lamp sources, this is accomplished via reflectance baffles integrated into the lighting fixtures. However, such baffles have an unintended consequence of reducing lamp efficiency.
New solutions using UVC LEDs provide increased design flexibility and safety for room occupants while being an inherently unidirectional and efficient light source. This directionality means that manufacturers can control the emission path without requiring additional baffles to redirect light. Moreover, these designs can place the UVC LED so it emits away from room occupants—allowing them to disinfect continuously without causing harm.
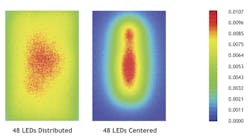
The compact nature of UVC LEDs also allows for more uniform disinfection in a room—regardless of shape or size. Traditional fixtures are constrained in design to the lamp's long tube housing. Such fixtures are necessarily placed in corners or along walls of a room for optimum UV radiant distribution. However, hot spots and cold spots are typical, especially in irregularly shaped rooms. Conversely, UVC LEDs can be placed in a grid-like pattern to accommodate room shape for maximum uniformity, providing an overall more efficient germicidal system. Figure 1 shows an example of two different optical patterns possible with the same set of UVC LEDs.
Because of the benefits of UV disinfection, hospitals are integrating surface and air disinfection systems into their protocols for combating HAIs. Laboratories that process suspected infectious disease samples may likewise benefit by augmenting their processes with UV disinfection. The product innovations made possible by UVC LEDs, combined with lessons learned from the hospital environment, will allow laboratories to further ensure the safety of their workers from LAIs.