Platelet function: beyond hemostasis—where does the lab fit in?
This is the tale of two entities—the clinical laboratory and the platelet. The clinical laboratory has been an essential tool in the detection, diagnosis, and management of disease for most of a century. As we move into the era of personalized or precision medicine, the role of the clinical laboratory is becoming ever more closely linked to the care of patients. Platelets and their functions can no longer be considered exclusively tied to hemostasis, or limited to a day shift specialty lab. The number and manner of ways platelets behave has yet to be finalized.
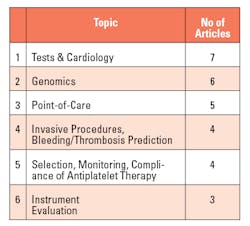
Table 1. (left) Top platelet function categories, Figure 1. (right) Platelets: traditional lab analyses3.
In the March 2013 issue of MLO, I published an article entitled, “An overview of platelet function testing.”1 Since then, BioMedUpdater has sent me a series of reports on articles published that included key words in it. Each report contained a list of the top 20 citations. Six categories accounted for 29 of the 60 citations (Table 1). Each of these categories challenges the clinical laboratory to change the nature, scope, availability, purpose, and location of platelet-related tests and requires the laboratory to form new and close relationships with clinical colleagues from very different specialties than those that have long been established.
When Dr. Gus Born developed a functional test for platelets and proposed its use for measuring their response to drug therapy 63 years ago, and electron microscopy revealed their anatomy, we were content to count platelets, and we had yet to understand and embrace functional tests. Schaef-Johns summed up the state of contemporary functional tests recently: “There is no perfect platelet function test…..Except for light transmission aggregometry, no tests are endorsed by platelet function testing experts.”2 (Figure 1).
Generally speaking: the evolving lab
During the 20th century the clinical laboratory test menu grew to more than 3,000 tests and became the driver of over 70 percent of clinical decisions.4 Laboratories excelled at providing data to clinicians and, with few exceptions, left it to the clinician to figure out what the data meant and how best to use it. Near-patient tests were developed; however, the efficacy and value of many such tests have yet to be realized. The underlying message was obscured by technical limitations, overstated advertisements,5 and, sometimes turf and political squabbles. There were—and still are—unmet medical needs (Table 2).
More and more people are realizing, however, that this must change. Laboratories must evolve beyond their traditional areas of expertise by integrating and harmonizing the services of 20 or more semi-independent specialties and absorbing formerly non-laboratory specialists, services and functions into a single, highly capable and efficient patient care service.
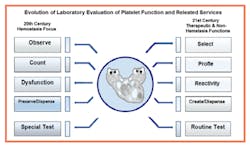
In just the last 10 years, advances in genomics, molecular and vascular biology, drug discovery, and targeting have revealed unmet medical needs in a number of specialties that can only be addressed by the clinical laboratory. The next generation of medical laboratory physicians and scientists will need to apply existing and new technologies to change from the current one-size-fits-all medical model to one that is tailored to patients based on their status and condition. The role of the clinical laboratory is changing. And, it needs to. As (Figure 2) shows, the time for passively providing volumes of accurate test results has passed. The 21st century clinical laboratory must position itself to provide entirely new kinds of information, services and therapeutic products.
Figure 2. Evolution of laboratory evaluation of platelet function and related services
More specific: new roles for platelets
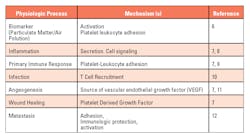
Platelet testing is an excellent case in point. At least seven non-hemostatic roles for platelets have now been identified. (Table 3). Others are likely to be discovered, and some of these non-hemostatic platelet functions can be attenuated with antiplatelet drugs, expanding the applications of these drugs to non-traditional uses. For example, in the case of a systemic infection, an antiplatelet drug may be used to modulate platelet recruitment of T cells, allowing antibiotic therapy to resolve the infection.
Table 3. Examples of known non-hemostatic functions of platelets
Going forward, platelets will need genomic and function profiles. Latent and residual reactivity measurements will be routine, and progenitor stem cells or even “designer” platelets will have to be created and provided by the laboratory.So, where are we at the moment? We have, as Dr. Barry Coller has said, just witnessed the golden age of platelet research.13 The most significant limitations in detecting and diagnosing heritable platelet disorders are awareness and test availability. Disease management continues to improve. Therapeutic advances based on genetic and stem cell technologies are in late-stage development, being tested in animal models, with some now moving to the clinical trial stage. For example, Wiskott-Aldrich syndrome has been reversed using gene therapy at Boston's Children's Hospital.14
Unmet medical needs for actionable genomic, functional and pharmaco-responsiveness information about platelets continues to grow and are fueled by the expanding role of antiplatelet therapy, including dual and triple antiplatelet therapy. Companion diagnostic tests may help develop patient-specific treatment protocols, and guide antidote therapy as well.
The perfect test for platelet function does not exist. There is no single test that can assess the range of platelet functions in hemostasis and non-hemostasis processes. An array of genomic and functional tests will be needed, as will patient response tests for safety, tolerability and efficacy. Transfusions of type specific and HLA matched platelets will be replaced by designer platelets—platelets made to order by the laboratory for a specific patient.
Precision medicine: the wave of the present
The foundation for precision medicine is the clinical laboratory, and it must lead the way in developing, implementing, and providing services and products for precision medicine. That means it is time for laboratories to agree on the basics: establishing procedural guidelines and implementing proficiency testing programs; standardizing specimens types and collection procedures, sample preparation, wavelengths, incubation times and temperatures; stirring speeds; test times; reagent concentrations; reported parameters, etc.—all of which remain inconsistent at the moment. That is where we need to start so that the clinical lab is prepared to be fully integrated into the precision medicine model. The answer to the question posed in the title: where does the lab fit in? Everywhere. And platelet testing is a poster child for the precision lab that is emerging and will continue to in the years ahead.
References
-
Trolio WM. An overview of platelet function testing. MLO. 2013;45(3):30-31.
-
Schaef-Johns G. Clopidogrel platelet function tests: caveats and controversies. Hot Topics. Mayo Clinic. Department of Laboratory Medicine and Pathology. Jacksonville, FL. Dec 2011.
-
White JG. Electron Micrograph. Circa 1969. (with permission)
-
Forman RW. Why is the laboratory an afterthought for managed care organizations? Clin Chem. 1996;42:813–816.
-
Krumholz HM. Examining an ad for a platelet inhibition test. www.cardioexchange.org/voices/examining an ad for a platelet inhibition test/. 27 Feb 2011. New England Journal of Medicine.
-
Delfino RJ, Staimer N, Tjoa T, et al., Circulating biomarkers of inflammation, antioxidant activity and platelet activation are associated with primary combustion aerosols in subjects .with coronary artery disease. Environ Health Perspect. 2008;116(7):898–906.
-
Brass L. Understanding and evaluating platelet function. ASH Education Book. (12/4/2010) Vol. 2010 No. 1. 387-396.
-
Fuentes QE, Fuentes QF, Andrés V, Pello OM, Font de Mora J, Palomo GI. Role of platelets as mediators that link inflammation and thrombosis in atherosclerosis. Platelets. 2013; 24(4):255-262.
-
Ware J, Suva LJ. Platelets to hemostasis and beyond. Blood. 7 April 2011. Vol.117, No. 14, 3703.
-
Zarbock A., Polanwska-Grabowska, RK, Ley K. Platelet-neutrophil-interactions: linking hemostasis and inflammation. Blood Reviews. doi:10.1016/jblre.2006.06.001.
-
Ferrer-Acosta Y, Gonzales M, Fernandez M, Washington V. Emerging roles for platelets in inflammation and disease. J Infect Dis Ther. 2014;2:4.
-
Egan K, Crowley D, Smyth P, et al. Platelet adhesion and degranulation induce pro-survival and pro-angiogenic signaling in ovarian cancer cells. PLoS ONE. 6(10) e26125. doi: 10.1371/journal.pone.002125.
-
Coller BS. Historical perspective and future directions in platelet research. J Thromb Haemost. 2011; Jul. 9 (Suppl 1): 374-395.
-
Ulrich T. Gene therapy gets in the ring with another disease (Wiskott-Aldrich syndrome). Vectorblog.org/2014/05/gene-therapy-gets-in-the-ring-with-another-disease/ © Boston Children's Hospital, 2005-2015. William M. Trolio, BS, MT, CLT, MBA, FBA, is Vice President and Chief Science Officer for Pennsylvania-based Bio/Data Corporation.