Emerging approaches to the examination of lipoproteins for cardio-metabolic risk stratification
Cholesterol has important functions in the body, including serving as a precursor for all steroid hormones and bile acids. Excess accumulation of esterified cholesterol, as part of dyslipidemia, in the walls of arteries results in the formation of fatty streaks. Fatty streaks can further develop into plaques. Formation of plaques in the heart may lead to premature atherosclerosis and coronary artery disease (CAD), while formation of plaques in vessels of the brains can lead to cerebrovascular disease. Plaque formation in the arteries of the arms and legs may lead to peripheral vascular disease.1
Lab measurements of lipids play an important role in identifying cardiovascular risks in individuals. Elevation of various biomarkers such as total cholesterol (TC), low density lipoproteins (LDL), and triglycerides (TG) and decreased levels of high density lipoproteins (HDL) all contribute to the development of atherosclerosis.1
In patients with CAD, recent clinical trials show the need to adjust LDL levels to even lower levels to prevent recurrent CAD. LDL levels show just an incomplete sign of atherogenic potential.2 LDL commonly is reported by the Friedewald equation (LDL = TC –HDL-TG/5). This equation will yield inaccurate results in patients with high triglycerides levels (greater than 400 mg/dL), or in patients who are not fasting.3 One way to circumvent the issues with the LDL calculation method is the use of homogenous, or “direct” assay, for LDL determination. Recent studies, however, show that the use of such methods is unsuitable in a dyslipidemic population.4
Lipoprotein analysis is an essential procedure for the cardiovascular risk assessment. The focus has been on testing only the routinely measured lipoproteins such as low density and high density lipoproteins, plus testing for total cholesterol and triglycerides. These routine lipid profile measurements, however, do not include determination of various lipoprotein subfractions.1
Routine lipoprotein testing, therefore, might not be the best strategy for at risk patients, such as those with cardiovascular disease or diabetes.5 This article seeks to shed light on the need to include additional and unique testing parameters in the lipid profile measurements.
The traditional cholesterol panel
The difference between total cholesterol and HDL concentration is called non-HDL. Non-HDL is a novel idea that is an estimate of cholesterol content in the atherogenic lipoproteins, including intermediate-density lipoprotein (IDL), very low density lipoprotein (VLDL), LDL, and lipoprotein cholesterol Lp(a). Non- HDL has been recognized to be superior over LDL for measuring risks for vascular events. As part of its national lipid treatment guidelines, the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATPIII) has included non-HDL as a secondary goal of therapy. In addition, the American College of Cardiology and the American Diabetes Association guidelines have noted the importance of non-HDL as a major goal therapy for lipoprotein management in patients at risk for cardiovascular events.6
The routine lipid panel that is ordered for cardiovascular assessment includes TC, LDL, HDL, and triglycerides. Several potentially valuable adjuncts to the standard panel are emerging as additional lipid parameters. Alternate atherogenic particles such as LDL particle number, apoB, non-HDL, and apolipoprotein A-1, which is the major protein of HDL, are being identified.6-8
Due to the heterogeneous composition of LDL particles and atherogenic nature of small dense LDL, LDL plasma cholesterol levels do not necessarily reflect the exact and complete extent of lipid abnormality. As an example, type 2 diabetes patients often have hypertriglyceridemia and increased apoB levels, which are atherogenic factors, despite low or normal plasma levels of LDL cholesterol.9 Blood plasma concentrations of Lp(a) have been shown to be an independent risk factor for CAD. Indeed, increased levels of Lp(a), more than 30 mg/dL, contribute to an increased risk of stroke and premature CAD.1, 10
While LDL and HDL cholesterol levels are already known risk factors, apoB, apoA1, and apoB/apoA1 ratio should be regarded as highly predictive factors in the assessment of cardiac risk as well. In particular, ApoB in individuals who have normal or low concentrations of LDL cholesterol will be helpful for the diagnosis in individuals with common lipid abnormalities.7 At present, however, most of these parameters have had utility only in the research field.6-8
Determination of LDL is the primary target for the risk assessment and prevention of CAD. LDL is made up of three components: Real LDL (R-LDL), IDL, and Lp(a). R-LDL = Total LDL (T-LDL) – Lp(a) – IDL. R-LDL subclasses are directly measured as LDL1, LDL2, LDL3, and LDL4. Lp(a) and IDL are more atherogenic than R-LDL. Based on size and density, two R-LDL patterns have been identified. R-LDL pattern A is large, buoyant LDL and is least dangerous. Like oxidized LDL, R-LDL pattern B, which is small and dense, is most dangerous.11 LDL, as derived from the standard calculations, is not accurate in the case of high triglyceride levels above 400 mg/dL in the blood. In addition, a panel of NCEP has recommended that better and more accurate tests should be used for routine diagnostic procedures, such as methods that separate out LDL directly for cholesterol quantitation.1,12
HDL, on the other hand, has protective properties such as removal of cholesterol from cells through a reverse cholesterol transport pathway, prevention of endothelial dysfunction, and inhibition of platelet and factor X activation.13 HDL exists in a disk shape, or more commonly, a spherical shape. Two major forms of spherical HDL are HDL subtypes HDL2 and HDL3. HDL2, which makes up the majority of the HDL, is larger than HDL3 subtype. HDL2 is also more protective than HDL3 for CAD risk. Furthermore, lipid drugs have a differential effect on the level of HDL subtypes.14 VLDLs are the main carriers for liver-derived (endogenous) triglycerides. Furthermore, excess dietary intake of trans fats, saturated fatty acids, and carbohydrates increases the production of VLDL.1 Small VLDL, IDL, ApoB, and ApoCII, measured in fasting individuals, can present a risk factor for the progression of CAD and atherosclerosis.15 VLDL remnants, also referred to as IDL, are usually present during the conversion of VLDL to LDL and do not accumulate in the plasma in fasting individuals; however, in patients with certain types of hyperlipoproteinemia, elevated levels can be seen in blood plasma.1 ApoB is seen in VLDL, IDL, and LDL, and its increased levels are associated with CAD.16
Moreover, the role of triglycerides-rich lipoproteins as a primary risk factor in patients at high risk for CAD has been established.17 Increased glycerides levels in the blood, increased LDL cholesterol, and LDL/HDL ratio beyond 5, along with hypertriglyceridemia, have been shown to increase CAD risk by several folds.18 Therefore, lipoprotein-rich triglycerides such as small VLDLs and IDL are associated with atherosclerosis and CAD. Subclasses of VLDLs such as VLDL3 are more atherogenic. Triglyceride-rich lipoprotein remnants such as VLDL, IDL, lipoprotein B, and apolipoprotein CIII (apoC-III) are related to the progression of CAD. In particular, apoC-III in VLDL subclasses that are denser and smaller are associated with CAD.15.19
The direct-measured lipid panel
Various guidelines recommend a comprehensive approach to identify patients at risk for cardio-metabolic risk stratification.5,20,21 Unlike the traditional cholesterol panel (Table 1), the vertical auto profile (VAP) test is a direct-measured lipid panel. VAP tests are used for comprehensive lipid analysis and simultaneous determination of cholesterol concentration for all five lipoprotein classes and subclasses. The VAP test directly measures LDL. It is also accurate in non-fasting individuals, unlike calculated LDL, which could be low in patients who do not fast as directed prior to testing.12 Furthermore, the VAP test provides measurements of various lipid components including HDL, TC (VLDL), non-HDL, apolipoprotein B100 (apoB100), Lp(a), IDL, LDL-R, LDL-R subclasses, and remnant lipoproteins such as VLDL3, HDL2 and HDL3.12
Table 1. Reference ranges for selected lipids and lipoproteins for adults.24
The VAP test uses single vertical spin, inverted rate zonal, and density gradient ultracentrifugation simultaneously to measure concentrations of cholesterol for all five lipoproteins LDL, VLDL, IDL, HDL, Lp(a), and subclasses.23
The VAP procedure takes less than one hour to perform and involves the following steps: ultracentrifugation, enzymatic treatment, and software analysis. Ultracentrifugation involves a two-layer density gradient with the bottom layer having a 1:40 serum dilution, followed by centrifugation at 65,000 rpm, which is followed by cholesterol analysis using a continuous flow VAP cholesterol analyzer.22
In 1985, the National Cholesterol Education Program (NCEP) was launched by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health. NCEP has put together guidelines for the benefits of lowering cholesterol levels for the prevention of CAD. The NCEP ATP (III) guidelines include the following: 1) measurement of direct LDL; 2) non-HDL and metabolic syndrome (secondary targets of therapy); and 3) emerging risk factors such as Lp(a), small LDL pattern, HDL subclasses, lipoprotein remnants, and apoB. The VAP test complies with NCEP, ATP(III) guidelines.24,25
One advantage of the VAP test is that it measures additional classes of lipoproteins such as Lp(a), IDL, and also subclasses of LDL, HDL (HDL2 and HDL3) and VLDL subclasses (VLDL1,VLDL2,VLDL3). The routine and standard lipid panel testing consists of ordering total cholesterol, LDL, HDL, and triglycerides.6 By measuring additional lipid parameters, the VAP test can identify patients who are at high risk for CAD and who otherwise would not be identified through routine and standard lipid panel testing. 23
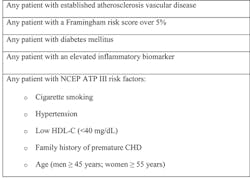
Various risk assessment tools or models have been developed for cardiovascular disease prevention. Examples of these models include U.S. Framingham risk score (FRS) and the European Systematic Coronary Risk Evaluation (SCORE). Age, gender, total cholesterol, LDL, HDL, smoking, systolic blood pressure, and diabetes are among the factors in the ATP(III) FRS. ATP(III) FRS, however, underestimates the total atherosclerotic vascular disease (Table 2).26
Table 2. Indications for seeking the VAP test.22
Lipid testing into the future
Lipid testing has come a long way and continues to evolve further. Analytical methods that are able to test various lipoprotein fractions and subfractions are essential for the detection of various lipid disorders. Measurement with a comprehensive lipid profile that includes specific and sensitive tests helps detect dyslipidemia and associated disorders earlier and more accurately, leading to better management of various cardiovascular disorders. Proper testing is a major factor for stopping the progression of CAD and lowering the burden of disease. Clinical laboratories should consider adding the lipoprotein subfractions discussed here to their future lipid test menu. Physicians should begin ordering such tests and evaluating these parameters.
1. Bishop ML, Fody EP, Schoeff LE. Clinical chemistry, techniques, principles, correlations (7th edition). Philadelphia, PA, Lippincott Williams & Wilkins, 2013.
2. Mudd JO, Borlaug BA, Johnston PV, et al. Beyond low-density lipoprotein cholesterol: defining the role of low-density lipoprotein heterogeneity in coronary artery disease. J Am Coll Cardiol. 2007 30;50(18):1735-1741.
3. van Deventer HE, Miller WG, Myers GL, et al. Non-HDL cholesterol shows improved accuracy for cardiovascular risk score classification compared to direct or calculated LDL cholesterol in a dyslipidemic population. Clin Chem. 2011;57(3):490-501.
4. Nauck M, Warnick GR, Rifai N. Methods for measurement of LDL-cholesterol: a critical assessment of direct measurement by homogeneous assays versus calculation. Clin Chem. 2002;48(2):236-254.
5. Brunzell JD, Davidson M, Furberg CD, Goldberg RB, Howard BV, Stein JH, Witztum JL. American Diabetes Association; American College of Cardiology Foundation. Lipoprotein management in patients with cardiometabolic risk: consensus statement from the American Diabetes Association and the American College of Cardiology Foundation. Diabetes Care. 2008;31(4):811-822.
6. Blaha MJ, Blumenthal RS, Brinton EA, Jacobson TA. National Lipid Association Taskforce on Non-HDL Cholesterol. The importance of non-HDL cholesterol reporting in lipid management. J Clin Lipidol. 2008;2(4):267-273.
7. Walldius G, Jungner I, Holme I, Aastveit AH, Kolar W, Steiner E. High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (AMORIS study): a prospective study. Lancet. 2001;358 (9298):2026-2033.
8. Saenger A. Cardiovascular Risk Assessment Beyond LDL Cholesterol: Non-HDL Cholesterol, LDL, Particle Number, and Apolipoprotein B. http://www.mayomedicallaboratories.com/articles/communique/2011/11.html.Accessed November 26, 2013.
9. Sniderman AD, Scantlebury T, Cianflone K. Hypertriglyceridemic hyperapob: the unappreciated atherogenic dyslipoproteinemia in type 2 diabetes mellitus. Ann Intern Med. 2001;18;135(6):447-459.
10. Craig WY, Neveux LM, Palomaki GE, Cleveland MM, Haddow JE. Lipoprotein(a) as a risk factor for ischemic heart disease: metaanalysis of prospective studies. Clin Chem. 1998;44(11):2301-2306.
11. Carmena R, Duriez P, Fruchart JC. Atherogenic lipoprotein particles in atherosclerosis. Circulation. 2004;109(23 Suppl 1):III2-1117.
12. Bachorik PS, Ross JW. National Cholesterol Education Program recommendations for measurement of low-density lipoprotein cholesterol: executive summary. The National Cholesterol Education Program Working Group on Lipoprotein Measurement. Clin Chem. 1995;41(10):1414-1420.
13. Viles-Gonzalez JF, Fuster V, Corti R, Badimon JJ. Emerging importance of HDL cholesterol in developing high-risk coronary plaques in acute coronary syndromes. Curr Opin Cardiol. 2003;18(4):286-294.
14. Morgan J, Carey C, Lincoff A, Capuzzi D. High-density lipoprotein subfractions and risk of coronary artery disease. Curr Atheroscler Rep. 2004;6(5):359-365.
15. Hodis HN. Triglyceride-rich lipoprotein remnant particles and risk of atherosclerosis. Circulation. 1999; 99(22):2852-2854.
16. Olofsson SO, Borèn J. Apolipoprotein B: A clinically important apolipoprotein which assembles atherogenic lipoproteins and promotes the development of atherosclerosis. J Intern Med. 2005;258(5):395-410.
17. Chapman MJ, Ginsberg HN, Amarenco P, et al. European Atherosclerosis Society Consensus Panel. Triglyceride-rich lipoproteins and high-density lipoprotein cholesterol in patients at high risk of cardiovascular disease: evidence and guidance for management. Eur Heart J. 2011;32(11):1345-1361.
18. Cullen P. Evidence that triglycerides are an independent coronary heart disease risk factor. Am J Cardiol. 2000;86(9):943-949.
19. Fujioka Y, Ishikawa Y. Remnant lipoproteins as strong key particles to atherogenesis. J Atheroscler Thromb. 2009;16 (3):145-154.
20. Jellinger PS, Dickey RA, Ganda OP, et al. AACE Lipid Guidelines Committee. AACE medical guidelines for clinical practice for the diagnosis and treatment of dyslipidemia and prevention of atherogenesis. Endocr Pract. 2000;6(2):162-213.
21. Grundy SM, Cleeman JI, Merz CN, et al. National Heart, Lung, and Blood Institute; American College of Cardiology Foundation; American Heart Association. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227-239.
22. Atherotech Diagnostics Lab.The VAP Lipid Panel. http://www.atherotech.com/VapCholTest/default.asp.Accessed November 26, 2013.
23. Kulkarni KR. Cholesterol profile measurement by vertical auto profile method. Clin Lab Med. 2006; 26(4):787-802.
24. ATP III At-A-Glance: Quick Desk Reference. National Heart, Lung, and Blood Institute. http://www.nhlbi.nih.gov/guidelines/cholesterol/atglance.html. Accessed November 11, 2013.
25. Analytical performance of the cholesterol profile measurement by Vertical Auto Profile [VAP]: analysis of NCEP III guidelines lipid analytes. http://www.atherotech.com/images/vapliterature/pdfs/vapaccuracywhitepaper_20110831.pdf. Accessed November 26, 2013.
26. Ton VK, Martin SS, Blumenthal RS, Blaha MJ.Comparing the new European cardiovascular disease prevention guideline with prior American Heart Association guidelines: an editorial review. Clin Cardiol. 2013;36(5):E1-6.