Clostridium difficile infection: the importance of accurate diagnosis
Broad-spectrum antibiotic treatment can lead to diarrhea in certain patients. Clostridium difficile is the most common cause of antibiotic-associated diarrhea. Bacteria of the genera Clostridia are gram-positive, obligate anaerobes that include C. tetani, C. perfringes, C. botulinum, and C. difficile. These bacteria have the capacity to form spores that are resistant to heat and most disinfectants, which contributes to their efficient transmission. Clostridia can also produce various toxins that play a major role in the pathogenesis of the diseases that they cause.
Toxin-producing strains of C. difficile (toxigenic C. difficile) can cause antibiotic-associated diarrhea, whereas non-toxigenic C. difficile are non-pathogenic. C. difficile can be found in the intestine of up to 5% of individuals. Prolonged hospitalization and residence in a long-term care facility increase the likelihood of both colonization as well as the generation of C. difficile disease. Broad spectrum antibiotic usage and other conditions that alter the normal composition of intestinal flora also predispose to the acquisition and overgrowth of C. difficile and to the development of C. difficile infection (CDI).
Disease
CDI is a disease of the large intestine, and the severity ranges from uncomplicated diarrhea to severe colitis that can result in life-threatening toxic megacolon.1 The pathogenesis of CDI primarily involves two bacterial toxins: toxin A, which is an enterotoxin that affects the permeability of the colonic epithelial layers; and toxin B, a cytotoxin that interferes with the regulation of cellular cytoskeletal proteins.2,3 CDI affects the most vulnerable patients, such as the elderly and immunocompromised patients, when they are treated for serious infections with antibiotics. Treatment modalities for CDI can be found elsewhere, and there are many reports concernng the ongoing challenges associated with treatment and management of CDI, especially with regard to cases of fulminant disease and recurrent CDI.4
Based on recent reports, both the incidence and severity of CDI are increasing.5 CDI has become one of the most common hospital-acquired infections and causes or contributes to a significant number of hospital-based deaths. In addition, hypervirulent strains that produce more toxin due to disruptions in the toxin regulatory elements have been associated with more severe disease in some studies as well as with more efficient transmission.6 There is an urgent need, therefore, to better control the spread of this infection in hospitals and in long-term care facilities. This article will focus on the role of detection methods in the accurate identification of cases of CDI and the consequences of inaccurate test results.
Diagnosis
Accurate diagnosis of C. difficile is essential for physicians to properly manage patients with antibiotic-associated diarrhea and for hospitals to effectively identify and control outbreaks of CDI. As with all diagnostic testing, it is critically important for clinicians to select patients for testing based on good clinical acumen.7 C. difficile testing should only be performed on at-risk patients with diarrhea as evidenced by multiple loose stools.8 Algorithms used by laboratories to identify the presence of toxigenic C. difficile have been continually evolving, and the organism and the disease are constantly changing. Fortunately, diagnostic methods are becoming more accurate and more facile, allowing for more rapid and precise identification of CDI.
There are many diagnostic methods available to detect toxigenic C. difficile in the stool of patients suspected of having CDI. Traditionally most tests have focused on the detection of C. difficile toxins A and B. Cytotoxicity in cell culture that is neutralized by antitoxin-containing antisera (CCNA) is considered the reference method for toxin B detection.9 Stool culture for C. difficile with confirmation of toxin production (toxigenic culture) is considered the gold standard for definitive identification of CDI, but it is generally impractical for clinical diagnosis due to the length of time before a result is generated.1,10 Immunoassays for the detection of toxin A and B have been a commonly used method to assist in the diagnosis of CDI because of their rapid turnaround time and ease of use in comparison with culture-based methods. These assays have been developed in various formats ranging from moderately complex enzyme-linked immunoassays to CLIA-waived lateral flow assays, allowing for a convenient option for many laboratories. All of these toxin immunoassays, however, have been associated with relatively low sensitivity and less than optimal specificity, resulting in poor negative and positive predictive values.
To address this issue, some manufacturers have added immunoassays for the detection of glutamate dehydrogenase (GDH) to their products.11-13 GDH is present in all strains of C. difficile, but is not specifically associated with toxigenic strains and as such lacks specificity, and additional testing must be done to identify toxigenic C.difficile. Furthermore, a GDH-positive but toxin-negative result identifies a potentially false negative due to the lower sensitivity of the toxin immunoassay, which then warrants follow up with a definitive confirmatory test.14,15 Several more recent reports, however, also question the sensitivity of GDH and suggest that a significant number of GDH-negative results might be C. difficile positive by other methods.16
The need for improved accuracy has promoted the development of molecular assays for the detection of pathogenic C. difficile in diarrheal stool samples. These assays are based on DNA amplification techniques that detect various conserved regions of the pathogenicity locus present in all known toxigenic C. difficile strains. There are a number of commercially available molecular tests, and they generally all have high sensitivity and specificity when compared to toxigenic culture and high percent positive and negative agreement when compared with one another.17-20 Many of the molecular tests are based on real-time PCR and are relatively complex and/or expensive. More recently, some FDA-cleared tests that are based on isothermal DNA amplification technologies, such as loop-mediated isothermal amplification (LAMP) and helicase-dependent amplification (HDA), have been developed.21 These tests are less complex and less expensive because they do not require a thermocycler or fluorescence reader. Certain tests do not require instrumentation, which reduces capital equipment budgets and makes the tests more accessible to smaller hospital laboratories. These new isothermal molecular tests offer laboratories that currently are using toxin immunoassays the benefit of the high level of accuracy of a molecular test without having to incur the significantly higher costs associated with complex instruments and a highly trained molecular staff.
It is imperative that both physicians and infection control specialists appreciate the pros and cons of the various diagnostic tests for C. difficile. Low sensitivity of an assay will lead to missed diagnoses. This can be detrimental to the patient, by delaying appropriate treatment. It also can be detrimental to the hospital, because often patients are not isolated or are inappropriately removed from isolation after a false negative test result—which can lead to further spread and more cases of CDI. Additionally, low specificity results in more false-positive cases in patients who may subsequently have necessary antibiotics curtailed and receive unnecessary treatment for CDI.
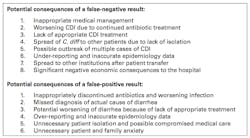
Table 1 lists some of the major consequences of the inaccurate diagnosis of CDI. Although diagnostic accuracy is always a goal in clinical and laboratory medicine, for CDI the consequences of a wrong diagnosis not only affect patient management, but have serious epidemiological and economic implications for healthcare facilities because of the importance of hospital-acquired infections. A single missed diagnosis can have widespread negative consequences beyond the affected patient’s outcome. Multiple missed diagnoses throughout the year can greatly expand the health and economic burden for a community.
There are an increasing number of reports that support the use of molecular testing upfront to minimize the number of incorrect test results following testing for CDI.22 It has been argued that the increased costs associated with using molecular tests for all cases of suspected CDI are justified because of the long-term saving related to more accurate diagnosis. In addition, less costly and easier to use molecular methods make this approach even more compelling, and allow for a greater number of hospital labs to implement molecular testing.
Clostridium difficile is the most common cause of diarrhea associated with antibiotics, and C. difficile infection has become one of the most common hospital-acquired infections with rates that are now surpassing methicillin-resistant Staphylococcus aureus. Accurate diagnosis of CDI is critical not only for proper patient management, but to promote effective infection control in order to minimize the spread of C. difficile and thus reduce outbreaks. Increasing evidence suggests that new molecular tests are the most useful tools for aiding accurate and timely diagnosis. Prior to the advent of lower-complexity and lower-cost molecular testing, multistep algorithms employing toxin immunoassays, and reflexing negative results to more definitive tests, served a useful purpose. It is becoming increasingly apparent, however, that directly testing all samples with a molecular test is the most efficient and effective way to rapidly diagnose CDI.
The authors wish to acknowledge and thank their colleagues John Tamerius, and Tim Stenzel for carefully reviewing this manuscript.
References
- Bartlett JG, Gerding DN. Clinical recognition and diagnosis of Clostridium difficile infection. Clin Infect Dis. 2008;46(suppl 1):S12-18.
- Voth DE, Ballard JD. Clostridium difficile toxins: mechanism of action and role in disease. Clin Microbiol Rev. 2005;18(2):247-263.
- Huelsenbeck SC, May M, Schmidt G, Genth H. Inhibition of cytokinesis by Clostridium difficile toxin B and cytotoxic necrotizing factors–reinforcing the critical role of RhoA in cytokinesis. Cell Motil Cytoskeleton. 2009;66(11):967-975.
- Shannon-Lowe J, Matheson NJ, Cooke FJ, Aliyu SH. Prevention and medical management of Clostridium difficile infection. Bmj. 2010;340:c1296.
- Gerding DN, Muto CA, Owens RC Jr. Measures to control and prevent Clostridium difficile infection. Clin Infect Dis. 2008;46(suppl 1):S43-49.
- Loo VG, Poirier L, Miller MA, et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. NEJM. 2005;353(23):2442-2449.
- Dubberke ER, Han Z, Bobo L, et al. Impact of clinical symptoms on interpretation of diagnostic assays for Clostridium difficile infections. J Clin Microbiol. 2011;49(8):2887-2893.
- Katz DA, Lynch ME, Littenberg B. Clinical prediction rules to optimize cytotoxin testing for Clostridium difficile in hospitalized patients with diarrhea. Am J Med. 1996;100(5):487-495.
- Bartlett JG. Antibiotic-associated diarrhea. NEJM. 2002;346(5):334-339.
- George WL, Sutter VL, Citron D, Finegold SM. Selective and differential medium for isolation of Clostridium difficile. J Clin Microbiol. 1979;9(2):214-219.
- Gilligan PH. Is a two-step glutamate dehyrogenase antigen-cytotoxicity neutralization assay algorithm superior to the premier toxin A and B enzyme immunoassay for laboratory detection of Clostridium difficile? J Clin Microbiol. 2008;46(4):1523-1525.
- Sharp SE, Ruden LO, Pohl JC, Hatcher PA, Jayne LM, Ivie WM. Evaluation of the C.Diff Quik Chek Complete Assay, a new glutamate dehydrogenase and A/B toxin combination lateral flow assay for use in rapid, simple diagnosis of clostridium difficile disease. J Clin Microbiol. 2010;48(6):2082-2086.
- Quinn CD, Sefers SE, Babiker W, et al. C. Diff Quik Chek complete enzyme immunoassay provides a reliable first-line method for detection of Clostridium difficile in stool specimens. J Clin Microbiol. 2010;48(2):603-605.
- Larson AM, Fung AM, Fang FC. Evaluation of tcdB real-time PCR in a three-step diagnostic algorithm for detection of toxigenic Clostridium difficile. J Clin Microbiol. 2010;48(1):124-130.
- Schmidt ML, Gilligan PH. Clostridium difficile testing algorithms: what is practical and feasible? Anaerobe. 2009;15(6):270-273.
- Novak-Weekley SM, Marlowe EM, Miller JM, et al. Clostridium difficile testing in the clinical laboratory by use of multiple testing algorithms. J Clin Microbiol. 2010;48(3):889-893.
- Boyanton BL Jr, Sural P, Loomis CR, et al. Loop-mediated isothermal amplification compared to real-time PCR and enzyme immunoassay for toxigenic Clostridium difficile detection. J Clin Microbiol. 2012;50(3):640-645.
- Bruins MJ, Verbeek E, Wallinga JA, Bruijnesteijn van Coppenraet LE, Kuijper EJ, Bloembergen P. Evaluation of three enzyme immunoassays and a loop-mediated isothermal amplification test for the laboratory diagnosis of Clostridium difficile infection. Eur J Clin Microbiol Infect Dis. 2012;31(11):3035-3039.
- van den Berg RJ, Vaessen N, Endtz HP, Schulin T, van der Vorm ER, Kuijper EJ. Evaluation of real-time PCR and conventional diagnostic methods for the detection of Clostridium difficile-associated diarrhoea in a prospective multicentre study; part 1. J Med Microbiol. 2007;56:36-42.
- Deshpande A, Pasupuleti V, Rolston DD, et al. Diagnostic accuracy of real-time polymerase chain reaction in detection of Clostridium difficile in the stool samples of patients with suspected Clostridium difficile Infection: a meta-analysis. Clin Infect Dis. 2011;53(7):e81-90.
- Chow WH, McCloskey C, Tong Y, et al. Application of isothermal helicase-dependent amplification with a disposable detection device in a simple sensitive stool test for toxigenic Clostridium difficile. J Mol Diagn. 2008;10(5):452-458.
- Catanzaro M, Cirone J. Real-time polymerase chain reaction testing for Clostridium difficile reduces isolation time and improves patient management in a small community hospital. Am J Infect Control. 2012;40(7):663-666.