Allowable measurement error associated with quality management plans
Measurement error is unavoidable, ever-present, and random in its nature. It is also unpredictable, making naturally occurring measurement error uncontrollable. Predictable process error is considered systemic and therefore controllable. Quality control plans can be designed to manage tangible systemic error to a point that is physically achievable; however, random measurement error can only be identified by the probability of its presence.
A ± error exists in any single reported measurement result. A comprehensive quality control plan needs to at least be aware of the estimated probability for the influence of the unpredictable random measurement error even if it is not reported along with the single measurement result. Decisions about a patient’s health classification will be affected by the estimated ± random measurement error associated with the single reportable result.
The qualities that will be real or implied that are claimed to be associated with a single patient result should be declared prior to designing the quality assurance and quality control protocols. A list of anticipated quality claims for a single patient result may include, but are not limited to, correctly identifying a patient’s health status, the amount of uncontrollable ± measurement error that is estimated to exist with a reported result, the risk for patient mis-classification, and, if applicable, the possible risk for reduced reimbursement for targeted patient populations.
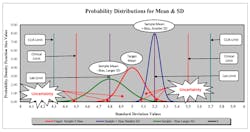
Understanding the nature of random and systemic measurement error and quantifying the estimates of bias and uncertainty will be critical to developing the objective evidence and communicating the confidence required for achieving the laboratory’s quality claims for a single reportable result. Random measurement error will take the form of a bell-shaped curve distribution and will represent the probabilities for uncertainty of an estimated central tendency of the random error. There will be an infinite number of bell curve shape representations that can be produced for each set of measurement data depending on the severity of disparate results that are obtained from the measurement function. A ± displacement of the bell curve probability space will indicate systematic error from a reference target.
Creating relational plots of the shape and displacement of the ± measurement error probability spaces will provide a way to visualize and quantify the required measurement performance that will be necessary to establish acceptable resolution of analyte concentration results. Multiple allowable ± measurement total error limit boundaries that are selected to reflect the local quality claims for reportable results can be superimposed onto the probability spaces in order to determine the risk probabilities for achieving any or all of the measurement quality goals. Figures 1 and 2 are general representations of this concept of measurement error, expressing typical probability distributions for mean and standard deviation (SD).
Refining the quality management of ± concentration measurement error and estimating the risk probabilities for identifying correct actionable patient health detection or patient health management decisions or for launching analytical correctional procedures, in response to a reportable result value, it would be reasonable and fair to extend the ± measurement total error concept to the acceptable ± quality limit boundaries. If a random measurement error probability space has been established for a particular clinically critical analyte concentration, then the acceptable quality limit boundaries should also reflect a measure of uncertainty similar to that of the measurement error probability space. This will create a method continuity in designing QA and QC procedures that will be scientifically consistent with the estimated measurement uncertainties.
Going from the theoretical to the practical, the Medicare Improvements for Patients and Providers Act, (MIPPA) has established a set of performance criteria for hemoglobin values that are considered acceptable for anemia management of end stage renal disease (ESRD) patients. The acceptable range for hemoglobin control for ESRD patient anemia management is between 10 g/dL to 12 g/dL. There is also a Medicare reimbursement incentive for achieving this clinical management goal for the anemia management of ESRD patients and a reimbursement deduction penalty for not maintaining ESRD patients within the 10 g/dL to 12 g/dL range. The Hgb range control scoring is weighted toward the 10 g/dL limit; Section 153 (c) ESRD Anemia Management Limits (Hgb). Medicare reimbursement for anemia management of ESRD patients can be reduced up to 2% for failing to achieve this clinical goal for Hgb.
With no ± allowable error distribution for the acceptable range limit points, 10 g/dL and 12 g/dL, the clinical goal and the reimbursement reduction risk resides within the Hgb measurement error and the ability to resolve an Hgb result of 10 g/dL and one of 9.9 g/dL. What is the laboratory’s ± total measurement error at a hemoglobin concentration of 10 g/dL? What kind of measurement error probability space is estimated from the ± random measurement error? How much ± bias is associated with the central tendency of the ± random measurement error probability space? How much of a risk is there for a reduction in Medicare reimbursement given the 10 g/dL limit point and the uncontrollable naturally occurring random measurement error of the hemoglobin methodology at 10 g/dL?
To analyze the Hgb methodology for its ability to accurately measure a 10 g/dL Hgb concentration, we must create a performance boundary that truly represents the ± measurement error that is present in the measurement process under normal operating conditions. Figure 3 illustrates the model for using a distributed allowable error limit probability space approach. In this example, the distributed allowable error boundary probability space is created by using the mean and SD of a known 10 g/dL Hgb concentration sampled several times under normal laboratory conditions. In this example, I use a mean of 10 g/dL and an SD of .06 to create the distributed allowable error limit probability space along with the 1, 2, and 3 SD limits for the distribution. The performance boundary cutoff probability space will now be more consistent with the existing Hgb methodology performance.
Given the unpredictable nature of random measurement error, I have plotted three different theoretical measurement error distributions for Hgb concentrations of 10 g/dL, 10.1 g/dL, and 9.9 g/dL. These theoretical result distributions are then compared to the distributed allowable error boundary probability space.
The first observation of the three theoretical result distributions is that there is poor resolution for a ± .1 g/dL difference in an Hgb concentration of 10 g/dL and 9.9 g/dL or 10.1 g/dL. Second, the 9.9 g/dL concentration, a result that would fail the MIPPA lower range limit, has a measurement error distribution, 9.9 g/dL ± .1, which would only exceed the -3 SD limit of the distributed allowable error limit probability space, 10.0 g/dL ± 3 SD (.18), at a cumulative risk of 21.19%. So, a 9.9 g/dL specimen could be indistinguishable from an actual 10.0 g/dL concentration at a cumulative risk of 78.81% of the time given the ± measurement error for hemoglobin that is present in both the 9.9 g/dL data and the 10.0 g/dL distributed allowable error limit probability space. There is a 42.07% chance to exceed the -2 SD limit of the 10.0 g/dL distributed allowable error limit probability space, which improves the resolution detection for the 9.9 g/dL concentration if a ± 2 SD limit is identified as the quality goal for the 10.0 g/dL distributed allowable error limit probability space.
If the risks for accurate patient health classification, patient anemia management, and Medicare reimbursement reduction become part of the laboratory quality claims for this example case of Hgb analysis, then controlling Hgb at 10 g/dL and 9.9 g/dL at a decision distribution that is concurrent with the Hgb methodology measurement error that is currently in use would make good quality sense. There also may be similar quality restrictions placed on additional analytes in the future. It would be good to anticipate these kinds of changes in quality assurance and quality control considerations.
For any laboratory measurement process, the ability to demonstrate the diagnostic quality for a single reportable result should be equal in scope and detail for which the act of measurement is intended. This means that if a single reportable result will be used to determine a medically actionable response, then the quality assurance and control systems need to be able to quantify the accuracy, measurement error, analytical resolution, and risk assessment for patient health classification, particularly at critical decision points for patient health determinations.
Completing the quality assurance/quality control loop, it would be appropriate to receive specific feedback from the recipients of the laboratory’s work products as to how their clinical commitment to their patients has been improved through the efforts of an improved quality assurance and quality control program by linking common quality goals for patient diagnostics and patient health management. A set of well-defined direct queries can be submitted to the laboratory’s end users. The responses from the end users can be scored as to their positive or negative outcomes to the queries and evaluated by their cumulative percentages in a Pareto chart. Following the Pareto principle that 80% of the effects of success or failure will be caused by 20% of all cited quality process categories, 20% of the total number of category query responses will have an 80% influence on the successful confirmation of the laboratory’s quality assurance and quality control programs or can assist in focusing on the more labor-beneficial areas of laboratory quality assurance and quality control improvement activities.
There are many additional factors that influence a single patient laboratory result. As knowledge increases about measurement error, patient biological variance, method capabilities, and new demands for diagnostic accuracy, more elements of quality assurance and quality control need to be considered that will accommodate these new interrelated and influencing factors. Quality is not automatic. It requires individual interest, participation, and the enthusiasm to improve with time.