Syringe reuse is a worldwide problem. So is accidental needlestick injury. Both problems could be dramatically reduced if all syringes were truly and effectively safety-engineered and designed to preclude reuse. In a sense, accidental needlestick injuries are reuse, albeit unintentional. Both intentional syringe reuse and needlestick injuries can transmit hepatitis B virus (HBV), hepatitis C virus (HCV), HIV, and many other bloodborne pathogens from a contaminated donor to a recipient. Because of the serious risks involved, there is a need to disable the injection (piston action) capability and skin piercing (needle) capability of syringes immediately after the initial use.
Reuse can occur when there is a lack of resources, when there is a lack of knowledge (about the consequences of reuse), and when a syringe’s design permits reuse (even if it is labeled “for single use only”). Needlestick injury can occur when syringes without engineered safety features are used, when ineffectively designed safety syringes are used, and when effectively designed safety syringes are used incorrectly, i.e., not according to instructions.
In developing countries, syringe reuse has been identified as a vector for the spread of disease. Unfortunately, needlestick injury data is often not collected, and needlestick injuries may be viewed as an unavoidable hazard in developing countries. In the United States and other developed nations, in the healthcare arena the needlestick injury problem outweighs the syringe reuse problem (although here, too, both problems exist). And, of course, in the illegal drug-use arena in any country, syringe reuse recurs with predictable frequency and deadly consequences.
Accidental needlestick injury
The World Health Organization (WHO) has estimated that worldwide more than three million people suffer accidental needlestick injuries each year.1 The U.S. Centers for Disease Control and Prevention (CDC) estimates that more than a half million sharps injuries occur in the United States annually, and approximately half of them (nearly 1,000 per day) occur in hospitals.2 Needlestick injuries are not limited to nurses and doctors, but also affect paramedics, ambulance drivers, law enforcement officers, correctional facility personnel, firefighters, sanitation workers, and others.1 Such injuries continue to be a serious problem in the U.S. and in other developed countries, as well as throughout the rest of the world, because effective safety-engineered syringes, which protect healthcare workers (and everyone else who might come in contact with contaminated syringes) from accidental needlesticks, are not universally used.
In November 2000 in the U.S., the Needlestick Safety and Prevention Act (NSPA; Public Law 106-430) was signed into law. In a letter to the editors of the New England Journal of Medicine earlier this year, Elayne K. Phillips, BSN, PhD, and colleagues from the University of Virginia, Charlottesville, noted:
It required employers to provide safety-engineered devices to employees who are at risk for exposure to bloodborne
pathogens, to include frontline workers in selecting these devices, to review exposure-control plans at least annually
to ensure that they reflect advances in sharps-safety technology, and to maintain sharps-injury logs that specify required
details about the injury.3
The impact of that federal legislation and its enforcement led to a reduction by approximately one-third in the number of needlestick injuries that are reported annually,4 but further change has come slowly,1 and hundreds of thousands of accidental needlestick injuries continue to occur each year in the U.S., exposing healthcare workers to potentially lethal or life-altering diseases.
Syringe reuse
WHO estimates that 40 percent of the more than 16 billion injections administered worldwide annually involve reused, unsterilized syringes and needles, with rates of unsafe injections climbing to 70 percent in some countries. The reuse of injection equipment is responsible worldwide for 33 percent of new HBV infections, 42 percent of HCV infections, and 2 percent of all new HIV infections. In South Asia, the WHO has estimated that unsafe injections are responsible for up to 9 percent of new HIV infections.5
In developing countries, used medical equipment is often reused, sold, or recycled because of its commercial value, frequently with no attempts, or ineffective attempts, to clean or sterilize these items. In recent decades, hundreds of people have contracted HIV because of syringe reuse in some nations that formerly were part of the Soviet Union, in Romania, in Libya, and elsewhere.
As previously mentioned, syringe reuse also occurs in the United States. Several years ago, when a spokesperson for a large manufacturer of conventional syringes was asked by a reporter about syringe reuse in the U.S., she replied, “The reuse issue does not exist in the United States.”6 Unfortunately, it does exist here, and reuse has happened again and again. A 1995 study published in the American Journal of Anesthesiology found that 39 percent of anesthesiologists reported having used the same syringe on different patients. A 2002 survey conducted by Cooper Research found that 1 in 100 healthcare providers surveyed admitted that they reused the same needle and/or syringe on multiple patients.
Instances of disease outbreaks as a result of syringe reuse have cropped up over the past several years in various states, including Connecticut (in 1997), New York (2001 and 2007), Nebraska (2002), Oklahoma (2002), Indiana (2007), and Nevada (2008). This phenomenon has occurred repeatedly, despite the medical profession’s mantra to “first, do no harm.”
The typical rationale in developing countries for syringe reuse is lack of resources (syringes or money for syringes). Many people in developing countries believe that any injection is vastly more potent than medicine taken orally. Often healthcare workers in developing countries have to grapple with the problem of a lack of resources, including an insufficient supply of syringes. In the U.S. and other developed countries, however, reuse cannot reasonably be attributed to a lack of resources.
A knowledge deficit is another oft-cited reason for syringe reuse. In developing nations, reuse certainly can be linked to insufficient knowledge or training; a lack of knowledge of the risks of reuse is also frequently found in developed countries such as the United States. In several instances of syringe reuse in the U.S., clinicians removed needles from syringes following use and replaced a contaminated needle with a sterile needle, under the erroneous belief that this somehow made the syringe safe for reuse. Disease risk from this practice is amplified when contaminated syringes are used to access medications in multidose vials. Once contaminated by a reused syringe and/or needle, multidose vials can harbor and spread disease regardless of the sterility of subsequent injection equipment. When medication is injected into intravenous fluids, a lapse in aseptic technique can contaminate intravenous access ports, lines, and/or fluids, resulting in serious bloodstream infections.
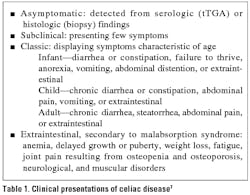
Acknowledging the impact of the factors discussed above (summarized in Table 1), the “elephant in the room”—by far the main reason for syringe reuse—is that most syringes are not designed to prevent their reuse. Their packaging and/or the syringes themselves may be marked “single use only” or “non-reusable,” but unless they are designed to preclude reuse, such warnings are often disregarded. First in the hierarchy of strategies to prevent reuse and needlestick injury must be engineering controls.
Some relevant history
The syringe was invented in 1853 by veterinary surgeon Charles Gabriel Pravaz and Dr. Alexander Wood.7 The basic design for most syringes has not changed substantially in almost 160 years. For more than a century, syringes were made of glass, and they were designed to be sterilized and reused. Doctors sterilized them before reuse by either immersing them in boiling water or by placing them in an autoclave.
In the early 1960s, a large syringe maker converted its manufacturing process from glass to plastic (thermoplastic),8 and the industry followed suit. Plastic syringes were promoted as being “disposable” and “single use,” even though the design was essentially the same as the design for reusable glass syringes. Plastic syringes cannot be adequately sterilized for reuse because plastic floats in water and because the heat from boiling water can soften and distort the shape of a plastic syringe. Also, many types of plastic cannot withstand the autoclaving process.
Auto-disable syringes are syringes that are designed to render themselves non-reusable after their first use. This can be achieved by any of several different designs. In some versions, the plunger locks or breaks, and in some the needle is retracted, either manually or automatically. However, many types of auto-disable syringes do not include any needle disabling/needlestick prevention feature. Contaminated needle and syringe combinations (even if the syringe plunger has been disabled) are a disease risk to healthcare workers and the community at large, especially in countries with limited or inadequate waste disposal systems.
The optimal solution
The best solution to the dual problem of accidental needlestick injury and syringe reuse is, of course, a syringe that is designed to prevent both. A syringe that offers the best and most effective solution is one that renders both the needle and syringe unusable, and prevents needle removal. Syringes with attached needle designs and automated retraction technology virtually eliminate the risk of a contaminated sharps injury to healthcare workers and others. Also, the automated retraction of the needle effectively precludes any reuse of the device. The attached needle design creates a “closed system” that reduces the possibility of infection9 and also further ensures the syringe’s non-reusability.
Syringes incorporating such designs represent a new paradigm in injection technology. The “one-size-fits-all” reusable syringe design is outmoded and creates unnecessary health risks to clinicians and patients. Injection devices must meet the demands of pandemic immunization programs as well as a scheduled allergy shot. A host of potential contaminants such as bloodborne pathogens and drug resistant microorganisms make single-use designs an imperative.
References
- Stoker R. Anatomy of a needlestick injury. Business Briefing: Global Healthcare – Advanced Medical Technologies. 2004;34,36,38. http://www.touchbriefings.com/pdf/950/stoker.pdf. Accessed October 16, 2012.
- Laramie AK, Davis LK, Miner C, et al. Sharps injuries among hospital workers in Massachusetts, 2010; Section: Massachusetts sharps injury surveillance system. Boston, MA: Massachusetts Department of Public Health Occupational Health Surveillance Program. http://www.mass.gov/eohhs/docs/dph/occupational-health/injuries/injuries-hospital-2010.pdf. Accessed October 17, 2012.
- Phillips EK, Conaway MR, Jagger JC. Percutaneous injuries before and after the Needlestick Safety and Prevention Act [A letter to the editor]. NEJM. 2012;366:670-671.
- Daugherty K. Needlestick statistics drop as passive safety device use rises. MLO. 2001;43(9) 39.
- World Health Organization. Injection safety, fact sheet No. 231. (Revised October 2006). http://www.who.int/mediacentre/factsheets/fs231/en/. Accessed October 23, 2012.
- Holding R. Deadly needles/syringes reused in U.S. despite risks, San Francisco Chronicle. Wednesday, October 28, 1998. http://www.sfgate.com/default/article/DEADLY-NEEDLES-Syringes-Reused-in-U-S-Despite-2982879.php. Accessed October 16, 2012.
- Lawrence G. The hypodermic syringe. Lancet. 2002;359(9311):1074.
- Becton Dickinson and Co. Celebrating the First One Hundred, 1897-1997. Franklin Lakes, NJ; 1997:69-71.
- Zule WA, Desmond DP, Neff JA. Syringe type and drug injector risk for HIV infection: a case study in Texas. Soc Sci Med. 2002;55(7):1103-1113.