As technology advances, laboratory decision makers are sometimes faced with the challenge of weighing the benefits of adopting a new or improved technology against the costs that doing so incurs. For the surgical pathology lab, that issue has come up with regard to voice recognition technology. Is it cost-effective to replace manual transcription with voice recognition software? Statistical analyses of data have provided an answer.
A double-blind study was conducted to determine annual costs and the return on investment for adding automated dictation to a busy histopathology department. Voice recognition in surgical pathology has received positive responses.1 However, questions have been raised: is this technology cost effective, and what is the time period for a return on investment? To answer these questions, our process improvement team enlisted the aid of experts to assist with this study.
Materials and methods
The study used comparable personnel in comparable surgical pathology departments. The surgical pathology personnel were of equal expertise and experience. Also, the specimens used ranged from complex to simple, and similar volumes were performed at two histopathology departments operated by one pathology group. One department used voice recognition (VR), and the other used manual transcription with dictation (MT).
A work flow for each technology was determined by the industrial engineering coordinator (Figures 1 and 2). A cycle time (CT) for each component of the work flow was collected for the pathology personnel performing each task. A timed study was made of the CT for the Pathologists’ Assistant (PA) grossing and the Pathologist’s microscopic dictation, and final diagnosis was later performed by an industrial engineering coordinator, as were additional cycle times in the workflow as a verification of the initial analysis of time study for each task. The annualized average costs for voice recognition (VR) and manual transcription with dictation (DT) were then determined.
Figure 1. Work flow utilizing dictation with manual transcription (MT) for the completion of a surgical histopathologic report with final diagnoses
Figure 2. Work flow utilizing voice recognition (VR) for the completion of a surgical histopathologic report with final diagnoses
Results
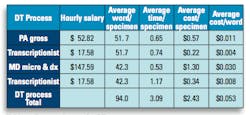
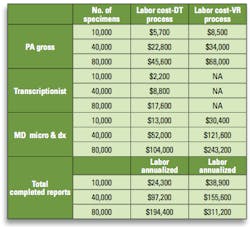
Once the cycle times for each component of the work flow cycles were collected, a comparable result was developed, called the average cost per word (CPW). The following equations were used for determination of the CPW and comparisons of the two technologies (Tables 1 and 2) and costs of a completed histopathological “specimen” report (Table 3):
Equations (Tables 1 and 2)
Average Word/Specimen = total words for all specimens/number of specimens
Average Time/Specimen = total time for all specimens/number of specimens
Average Cost/Specimen = salary (per minute) for each person performing a task x
Average Cost/Word = average cost/specimen ÷ average word/specimen
Labor cost for process = average cost/specimen x No. of specimens
Equations (Table 3)
Totals for completed reports:
DT = ACS for DT process total x No. of specimens
VR = ACS for VR process total x No. of specimens
Salaries used for the tables are for the Des Moines, Iowa, area utilizing human resource data and further comparisons with the www.Salary.com website. Annualized labor costs for a specific volume of “specimens” were determined from the data (Tables 1 and 2) and summarized (Table 3).
Table 1. Per word costs for DT process
Table 2. Per word costs for VR process
Table 3: Annualized costs comparing DT and VR processes based on work flow
Discussion
The work flow process maps and tables contain comparisons not previously reported. Our double-blind study did validate that the completion times for finalized reports, VR 2.21 min/specimen vs. DT 3.09 min/specimen, was shortened. The cost for this interval was a difference of $1.46 (VR $3.89 vs. DT $2.43). This cost differential resulted in the rejection of VR technology when annualized by Industrial Engineering criteria. The criterion for rejection is a calculated payback period of greater than five years, and in our situation payback would never occur.
The AWS, ATS, ACS, CPW and the annualized labor costs were calculated using simple ratios from cycle times and average salaries. The 42.3 AWS value for MD micro and dx in DT process (Table 1) was not timed in the initial study. This AWS value in Table 1 was based on a mathematic ratio from the PA data when a comparison of DT and VR grossing was performed on identical specimens from a preliminary study in preparation for our data collection. Therefore, a second cycle time study was performed to validate our data and compare timed events from two separate data collections. This second study showed a slightly shortened AWS; however the ATS was greater for the MD component. We concluded that the values of the mathematic ratio (initial) and the timed MD portion in the second study plus other data are comparable and did not significantly alter the annualized labor costs in Table 3.
Individuals who participated in this study had as close to identical credentials in anatomic pathology as possible to limit possible biases. Additionally, each technology was already established in each laboratory: VR had been in use for six months prior to the study, and DT had been in use for more than 20 years.
The variables that were known from the work flow process maps were considered prior to the collection of cycle times (CT) of each phase. A worksheet was developed for ease of collection of gross, microscopic, and transcription CT. This worksheet was then used by each individual for the collection of an entire day of timed tasks of each phase.
Another preliminary step was to compare the average number of words/specimen using both technologies prior to the collection of the CT. This was done by repeating several individual histopathology reports using both technologies of VR and DT on the same specimens, thus replicating the CT with both technologies on the same day. All specimens prosected and then finalized were randomized and of various complexities during the timed task phases. This study was also based on labor costs on similar daily volumes of specimens prosected at the two histopathology laboratories. The cycle times (CT) for addendums, pathologic staging, synoptic forms, diagnostic criteria, procedural disclaimers, and other items within a finalized surgical pathology report were purposely excluded from this study for purposes of clarity and ease of comparison.
Startup costs for equipment applicable in a “Return on Investment” (ROI) data analysis and those variables in an Excel file were purposely excluded. However, these costs were analyzed and compared from updated vendor estimates and actual costs of two VR technologies and one DT technology based on 10 licenses for each. This additional double-blind study again determined that the cost differences remained significant to reject VR as a replacement for DT despite the exclusion of other selected costs such as for computer hardware, updates for anatomic pathology software capable of word processing and installation of various components, wiring to the ten locations of the licenses, or necessary remodeling costs. The authors felt that inclusion of this data was not an integral component.
A next study that is planned by the authors is the return on investment comparing technologies from estimated and actual costs of manual transcription equipment, voice recognition equipment, software, and necessary remodeling costs when an entire histopathology department is renovated.
Conclusion
This comparative double-blind study between VR and DT was successfully completed after careful preparation and planning to limit biases. The advantages for VR are a shortened time for completion of reports and the ability to finalize reports without the aid or presence of ancillary staff. However, the cost to accomplish this is significant and ongoing, which leads to rejection of VR as a replacement for DT according to Industrial Engineering payback criteria.
Reference
- 1st Dragon. Online voice recognition solutions www.1st-dragon.com/Medical. Accessed June 26, 2012.
Appreciation to pathologists Jared Abbot, MD, PhD, and Larry Anderson, MD, and to medical transcriptionists Katie Powell, Susan Anthony, Catherine Munson, and Cindy Wheeler for offering suggestions and maintaining cycle times of their processes that guaranteed the success of this comparative study. Also gratitude to Piper Wall DVM, PhD, for her reviews and suggestions.
Contributors of this project were: Trent Shaner, MHS, PA(ASCP), Pathologists’ Assistant, Fellow (AAPA), and Timothy Drevyanko, MS, MD, Pathologist, Fellow (ABP), both of Iowa Pathology Associates; and Sue Burt, MT(ASCP), MS, Redesign Leader, and Julie Dotson, BBA, Process Improvement Coordinator, Clinical Quality, both of Iowa Health–Des Moines.