Comparing indirect fluorescent antibody assays to rapid diagnostic tests for the detection of influenza A(H1N1)pdm09
Accurate and rapid testing of patients for influenza virus is important to optimize antiviral use, minimize antibiotic use, and appropriately isolate hospitalized patients to prevent hospital-acquired infections. During the 2009 H1N1 pandemic, viral culture and real-time reverse transcriptase polymerase chain reaction (rRT-PCR) testing was available through public health laboratories and later through commercial laboratories. However, effective clinical management of patients hospitalized with respiratory illnesses often depends on timeliness of results.
CONTINUING EDUCATION
To earn CEUs, visit mlo-online.com and see this month’s test by clicking the CE menu item.
LEARNING OBJECTIVES Upon completion of this article, the reader will be able to:
- Determine appropriate testing methodologies to idenfity pandemic influenza.
- Compare and contrast the specificity and sensitivity of fluorescent antibody (FA) testing with rapid influenza diagnostic testing (RIDT) when testing for pandemic H1N1 influenza.
- Define and differentiate the six organisms commonly responsible for atypical pneumonia diagnoses.
- Compare and contrast the clinical challenges of diagnosing atypical pneumonia.
- Identify the role of molecular diagnostics in the determination of atypical pneumonias.
To help with initial diagnosis, many physicians utilized indirect or direct fluorescent antibody (IFA or DFA, respectively) or rapid influenza diagnostic tests (RIDT).Results of RIDT procedures are available within 30 minutes of specimen collection and do not require laboratory expertise, but reported sensitivity during the initial stages of the pandemic was low. Several studies looking at RIDT for detection of influenza A(H1N1)pdm09 have shown sensitivity ranging from 18% to 69%.1-11 IFA and DFA tests are performed in the hospital or reference laboratory, and results can be obtained within two to four hours. Additionally, because IFA and DFA tests are usually performed as part of a viral respiratory panel, they are useful for the identification of respiratory viruses other than influenza. Sensitivity of DFA for the detection of A(H1N1)pdm09 has been reported between 47% and 93%.1,3,6,9,11-16 Information is not currently available on the accuracy of IFA for the detection of A(H1N1)pdm09 in a clinical setting, although a newly developed H1N1-specific IFA claims to have up to 100% sensitivity.17,18 More information on the accuracy of IFA tests compared to other diagnostic methods for the detection of A(H1N1)pdm09 is needed to determine their utility in the diagnosis and management of patients with febrile respiratory infections.
Materials and methods
The Orange County Health Care Agency initiated enhanced surveillance for human cases of pandemic H1N1 on April 24, 2009. Clinicians and community partners were asked to report patients with influenza-like illness meeting certain epidemiologic criteria, which evolved over time based on Centers for Disease Control and Prevention (CDC) and California Department of Public Health guidance, and to submit specimens to the Orange County Public Health Laboratory (OCPHL) for testing. During the initial stages of the 2009 influenza pandemic, surveillance focused on case finding activities. Specimens were accepted at OCPHL if patient had influenza-like illness (ILI), defined as fever ≥ 100°F and cough and/or sore throat, and met one of the following conditions: 1) had contact with a confirmed case; 2) had traveled to areas with pandemic H1N1 activity in the seven days preceding illness onset; 3) had contact with someone with ILI who had traveled to areas with pandemic H1N1 activity; 4) had contact with pigs; 5) was part of a defined cluster or outbreak of people with ILI; or 6) was hospitalized with ILI or pneumonia.
Submission criteria were revised on June 25, 2010. Patients met the new criteria for testing if they had ILI, pneumonia, or severe, unexplained febrile respiratory illness, or sepsis-like syndrome (in infants, adults over 64 years of age, or persons with compromised immune systems) and met one of the following conditions: 1) was a healthcare worker; 2) was pregnant; 3) was part of a defined cluster or outbreak of people with ILI; 4) was hospitalized; 5) lived in an institutional setting.
Testing criteria were revised again on October 2, 2010, to focus on patients who were hospitalized in the intensive care unit or had died and had unexplained febrile respiratory illness, ILI, pneumonia or sepsis-like syndrome.Results were included in this analysis if rRT-PCR was performed through OCPHL; both rRT-PCR and either IFA and/or RIDT testing were performed for the same patient; specimens were collected on the same day, and the patient did not have a positive test for seasonal influenza. There were 638 specimens collected from April 27, 2009, through October 14, 2009, from 633 patients, that met these criteria.
Specimen types and testing methods
Specimens were received from hospitalized patients (70%), emergency room visits (17%), CDC Sentinel Provider Influenza Surveillance Program sites (10%), and outpatient visits (3%). Specimen types were known for 600 specimens and included nasopharyngeal or nasal swabs (256; 85%) and washes (322; 54%), tracheal aspirates (18; 3%), bronchoalveolar lavage (3; 0.5%), and lung tissue (1; 0.2%). Most (84%) of IFA specimens were nasal washes and the majority (68%) of RIDT specimens were nasopharyngeal swabs. Samples were taken at the point-of-care, and initial testing was done onsite or referred to a commercial laboratory. Additionally, samples were forwarded to OCPHL for confirmation by rRT-PCR using reagents and protocol provided by CDC (CDC Swine Influenza Virus Real-time rRT-PCR Detection Panel).
Each hospital supplied viral transport medium for specimens. Cool packs were used to maintain proper temperature of specimens during transport to OCPHL. Once received by OCPHL, specimens were placed in a refrigerator at 4°C ±2°C, then frozen to -70°C prior to extraction. All specimens were typed with InfA and InfB primers and probes. Influenza A positive specimens were sub-typed with seasonal H1 and H3 primers, and the CDC Swine Influenza Detection Panel was used to detect swine flu A and swine H1. All IFA testing was conducted at a hospital laboratory serving two hospitals using Bartels Viral Respiratory Screening and Identification Kit (Trinity Biotech,). RIDTs were performed at a variety of facilities and included QuickVue Influenza, which does not distinguish between A and B antigens (Quidel Corporation), QuickVue Influenza A+B, which distinguishes between A and B antigens (Quidel), and BinaxNOW Influenza A&B test (Inverness Medical).
Sensitivity and specificity were calculated using rRT-PCR for influenza A(H1N1)pdm09 virus as the reference. Test performance was determined for children (
Results
Two hundred forty-five specimens (38%) were positive for influenza A(H1N1)pdm09 (139 children/106 adults). There were 438 respiratory specimens taken from hospitalized patients, of which 131 (30%) were positive for A(H1N1)pdm09 (82 children/49 adults). Of the 200 specimens from non-hospitalized patients, 114 (57%) were positive for A(H1N1)pdm09 (57 children/57 adults). Median age of patients for whom specimens were included was 12 years (range:
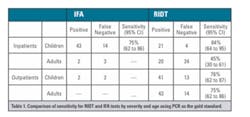
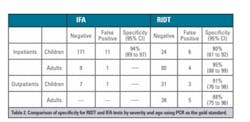
Overall sensitivity of IFA tests and RIDTs was 71% and 69%, respectively. Very few IFA results were received on adults and on outpatient children. Figure 1 and Table 1 present the sensitivity of RIDT and IFA tests by severity and age. Sensitivity of IFA and RIDT performed on hospitalized children was 75% and 84%, respectively. Sensitivity of RIDT for outpatient children was 76%. In comparison, sensitivity of RIDT performed on adults in outpatient settings was 75% compared to only 45% for hospitalized adults. Overall specificity was 91%. Figure 1 and Table 2 present the specificity of RIDT and IFA tests by severity and age. Specificity of tests performed on hospitalized children was 94% for IFA and 80% for RIDT. Specificity for RIDT performed in pediatric and adult outpatients was 91% and 88%, respectively. QuickVue Influenza A+B, the most commonly performed RIDT, had a sensitivity of 69% (CI: 60% to 77%) and a specificity of 96% (CI: 92% to 98%). Due to small numbers, sensitivity and specificity of QuickVue Influenza (non-A+B) and BinaxNOW A&B RIDTs are not displayed.
Figure 1. Sensitivity of IFA tests and RIDTs for the detection of pandemic H1N1 influenza. Sensitivity was calculated using real-time reverse transcriptase polymerase chain reaction as the gold standard. IFA results for other groups were not available due to lack of data
Mean time from illness onset to specimen collection was similar for hospitalized adults, (2.7 days) and outpatient adults (2.2 days) and was also similar for hospitalized children (2.8 days) and outpatient children (2.1 days), p>0.05. Mean age was significantly higher among hospitalized adults (52 years) compared to outpatient adults (31 years), p<0.05, and significantly lower among hospitalized children (5 years) compared to outpatient children (9 years), p<0.05.
Discussion
In choosing between RIDT and IFA tests, RIDT offers quicker results with similar sensitivity, requires less experienced personnel to perform, and utilizes less laboratory personnel time and equipment. However, IFA testing is often performed as part of a respiratory virus panel, and positive results for a different respiratory virus than influenza would provide useful information for infection control and other management decisions.
With such a low sensitivity, negative RIDT and IFA test results must be interpreted with caution. Since these tests produce a high number of false negative results, clinicians would not be able to rule out a diagnosis of influenza based on a negative result.
Sensitivity of RIDTs was lower in outpatient children (76%) compared to hospitalized children (84%) and was especially poor in hospitalized adults (45%) compared to outpatient adults (75%). Time from symptom onset to specimen collection was not significantly different among the various groups. We also looked at age as a possible factor affecting sensitivity. Hospitalized children were significantly younger than outpatient children, while hospitalized adults were significantly older than outpatient adults. It is well know that children shed more influenza virus and in greater quantities than adults. However, the effect of age on viral shedding in adults is less established. Clinicians should be aware that sensitivity of RIDTs varies greatly and may be poor in older adults.
The overall specificity of RIDT (91%) is similar to what has been reported in the literature for influenza A(H1N1)pdm09 (86% to 100%); however, results among certain subgroups and test types were much lower than expected.3,4,5,8,11,19,20 Since RIDT and IFA tests were performed in the clinical setting and PCR testing was performed at a different facility, it is possible that some RIDT and IFA tests were truly positive and the specimens lost integrity during transport to OCPHL. Given that PCR testing performed at OCPHL was used as the gold standard for disease classification, this would result in more false positives than is accurate due to misclassification of those who had A(H1N1)pdm09. While our results may be due to small sample size or loss of specimen integrity during transport, healthcare providers should be aware that these tests may produce false positives under certain conditions.
Our study is limited by the lack of detailed information recorded on specimen type (i.e., nasal swab v. nasopharyngeal swab) restricting our ability to account for different collection methods in our analysis. Additionally, in a small number of patients, the specimen tested by IFA or RIDT may not have been the exact specimen tested by rRT-PCR, although all specimens were collected on the same day. One hospital laboratory performed all IFA testing, while RIDT testing was performed in a variety of facilities and using different methods. Finally, since IFA and RIDT were performed at a different facility than rRT-PCR, storage or transportation issues (including transport temperature) may have affected the integrity of the sample and are limitations of the study.
In our study, clinically based diagnostic tests for influenza A(H1N1)pdm09 had variable sensitivities and specificities and may have led to false negative and false positive results. Treatment and infection control decisions should not be changed or delayed based on negative IFA or RIDT results. Research is needed to develop and validate more sensitive rapid testing for influenza.
References
- Hawkes M, Richardson SE, Ipp M, et al. Sensitivity of rapid influenza diagnostic testing for swine-origin 2009 A (H1N1) influenza virus in children. Pediatrics. 2010;25:e639-644.
- Louie JK, Guevara H, Boston E, et al. Rapid influenza antigen test for diagnosis of pandemic (H1N1) 2009. Emerg Infect Dis. 2010;16:824-826.
- Ginocchio CC, Zhang F, Manji R, et al. Evaluation of multiple test methods for the detection of the novel 2009 influenza A (H1N1) during the New York City outbreak. J Clin Virol. 2009;45:191–95.
- Centers for Disease Control and Prevention. Evaluation of rapid influenza diagnostic tests for detection of novel influenza A (H1N1) virus—United States, 2009. MMWR. 2009;58:826-829.
- Faix DJ, Sherman SS, Waterman SH. Rapid-test sensitivity for novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;13:728-729.
- Ganzenmueller T, Kluba J, Hilfrich B, et al. Comparison of the performance of direct fluorescent antibody staining, a point-of-care rapid antigen test and virus isolation with that of RT-PCR for the detection of novel 2009 influenza A (H1N1) virus in respiratory specimens. J Med Microbiol. 2010;59(Pt 6):713-717.
- Kok J, Blyth CC, Foo H, et al. Comparison of a rapid antigen test with nucleic acid testing during cocirculation of pandemic influenza A/H1N1 2009 and seasonal influenza A/H3N2. J Clin Microbiol. 2010;48(1):290–291.
- Centers for Disease Control and Prevention Performance of rapid influenza diagnostic tests during two school outbreaks of 2009 pandemic influenza A (H1N1) virus infection—Connecticut, 2009. MMWR. 2009;58(37):1029-1032.
- Miroballi Y, Baird JS, Zackai S, et al. Novel influenza A(H1N1) in a pediatric health care facility in New York City during the first wave of the 2009 pandemic. Arch Pediatr Adolesc Med. 2010;164(1):24-30.
- Uyeki T. Diagnostic testing for 2009 pandemic influenza A (H1N1) virus infection in hospitalized patients. N Engl J Med. 2009;361:e114.
- Landry ML. Diagnostic tests for influenza infection. Curr Opin Pediatr. 2011; 23(1):91-97.
- Leonardi GP, Mitrache I, Pigal A, Freedman L. Public hospital-based laboratory experience during an outbreak of pandemic influenza A(H1N1) virus infections. J Clin Microbiol. 2010;48(4):1189-1194.
- Landry ML, Ferguson D. Cytospin-enhanced immunofluorescence and impact of sample quality on detection of novel swine origin (H1N1) influenza virus. J Clin Microbiol. 2010;48(3):957-959.
- Bakerman P, Balasuriya L, Fried O, et al. Direct fluorescent-antibody testing followed by culture for diagnosis of 2009 H1N1 influenza A. J Clin Microbiol. 2011;49(10):3673-3674.
- Pollock NR, Duong S, Cheng A, et al. Ruling out novel H1N1 influenza virus infection with direct fluorescent antigen testing. Clin Infect Dis. 2009;49:e66-68.
- Sandora TJ, Smole SC, Lee GM, et al. Test characteristics of commercial influenza assays for detecting pandemic influenza A (H1N1) in children. Pediatr Infect Dis. 2009;J29:261-262.
- Higgins AD, Shaw CJ, Johnson JG, et al. Monoclonal antibody kit for identification of the novel 2009 H1N1 influenza A virus. J Clin Microbiol. 2010;48(8):2677-2782.
- Leonardi GP. Rapid identification of 2009 H1N1 influenza A virus using fluorescent antibody methods. Am J Clin Pathol. 2010;134(6):910-914.
- Uyeki TM, Influenza diagnosis and treatment in children: a review of studies on clinically useful tests and antiviral treatment for influenza. Pediatr Infect Dis J. 2003;22:164-177.
- Cruz AT, Demmler-Harrison GJ, Caviness AC, Buffone GJ, Revell PA. Performance of a rapid influenza test in children during the H1N1 2009 influenza A outbreak. Pediatrics. 2010;125:e645.
Sandra Okubo, MPH, and Michele Cheung, MD, MPH, are affiliated with Epidemiology & Assessment, Orange County Health Care Agency, Santa Ana, CA; Felice C. Adler-Shohet, MD, is affiliated with the Division of Infectious Diseases, Children’s Hospital of Orange County, Orange, CA.
Hildy Meyers, MD, MPH, affiliated with Epidemiology & Assessment, Orange County Health Care Agency, Santa Ana, CA, assisted the authors in the conception and design of the experiments. The experiments were performed by Kathryn Krusel, BS, affiliated with the Public Health Laboratory, Orange County Health Care Agency, Santa Ana, CA, and Kate Vogel, MA, affiliated with the Clinical Laboratory, Saint Joseph Hospital, Orange, CA. Ms. Krusel and Ms. Vogel also contributed reagents/materials/analysis tools. Ms. Okubo analyzed the data.
Citation: Nutter S, Cheung M, Adler-Shohet FC, Krusel K, Vogel K, et al. (2012) Evaluation of Indirect Fluorescent Antibody Assays Compared to Rapid Influenza Diagnostic Tests for the Detection of Pandemic Influenza A (H1N1) pdm09. PLoS ONE 7(3): e33097. doi:10.1371/journal.pone.0033097