In the early 1990s,
healthcare facilities across the country rushed to embrace a new
staffing experiment called decentralized phlebotomy. The trend to
dissolve the phlebotomy staff and reassign them as patient care
technicians (PCTs) or a similar appellation was gaining such a foothold
in the industry that one prognosticating author went so far as to
suggest “the phlebotomist now faces extinction,” and predict that by
2010 all venipunctures would be “performed by a team of patient care
technicians.”1,2
Please pass the ketchup; I would like to eat my
words.
What was I thinking? Here we are on the cusp of
2010, and not only is the phlebotomy profession not extinct, it is
alive, well, and flexing its biceps. For many facilities drawn to
decentralized phlebotomy Gold-Rush style, the promises did not pan out.
Perceived benefits included a more efficient workforce and higher
patient-satisfaction scores due to fewer individuals interacting with
the patient. Instead, it delivered contaminated blood cultures,
misidentified samples, skyrocketing specimen-rejection rates, friction
between the laboratory and nursing staff, and patient dissatisfaction
due to multiple venipuncture attempts and excessive bruising.
Most who tried the decentralized phlebotomy
concept ultimately found it to be vastly more difficult to implement
than perceived and returned blood-collection responsibilities to the
tried-and-true laboratory-based phlebotomist. But has decentralized
phlebotomy run its course? A recent online survey administered by the
Center for Phlebotomy Education asked its e-newsletter subscribers if
phlebotomy is centralized or decentralized in their facilities.
Sixty-one percent of those responding indicated specimen collection is
centralized in their facilities, whereas 39% reported a decentralized
system is in place where they work.
Reverting to lab-based phlebotomy
One of the many facilities evaluating a reversion
to laboratory-based phlebotomy is Augusta Health in Fishersville, VA.
According to American Society of Clinical Laboratory Scientists'
past-president Bernie Bekken CLS(NCA), MT(ASCP) BB, and program director
for Augusta's School of Clinical Laboratory Science, “We have had
decentralized phlebotomy for over 15 years, and it will be an adjustment
for the laboratory to start collecting inpatient phlebotomy again. Our
pathologists have discussed, for some time, the possibility of
relinquishing blood-collection responsibilities back to the laboratory.
It may happen as a restructuring of our patient-care model takes place.”
Bekken anticipates the transition will bring
about a significant reduction in costs of supplies, particularly with
regard to overuse of butterfly needles. “I can see this saving a lot of
costs for the organization,” he says. “I also expect to see a reduction
in hemolyzed samples, recollects, bruising, underfilled tubes, and
misidentified patients, and an increase in patient satisfaction and
safety.”
Bekken believes decentralized phlebotomy can work
when it is implemented correctly. “Decentralized phlebotomy is not
necessarily a bad thing. It depends on how much ownership non-laboratorians
take of the process. It worked for Augusta Health for 15 years because
our non-laboratory collection personal were trained comprehensively. You
cannot just teach them 'what' to do; you have to teach them the 'why.'
Also, the laboratory has to stay involved with the process. Our
laboratory has retained oversight of all errors with reports being sent
to nursing units each month as well as following up on corrective
actions.”
Even when it does work, decentralized phlebotomy
may not be cost effective. When one 304-bed hospital went from a
decentralized system back to centralized, it saved $400,000/year.3,4
In addition, the facility was able to post laboratory results on patient
charts two hours sooner than when samples were collected by a
decentralized workforce. Zwang, et al, reported that when non-laboratory
personnel collect blood specimens, it costs a hospital up to $1.8
million per year and results in up to 2,200 extra [patient] hospital
days per year.5
Drawing blood cultures in a decentralized
environment seems to be among the most costly downside to decentralizing
phlebotomy. Researchers in one study found hospitals incur a cost of
$8,720 per contaminated blood culture and an increase in the patient's
length of stay as a result of contaminated blood cultures of 4.5 days.
By using phlebotomists instead of emergency-room personnel to collect
blood cultures in the emergency department, the facility involved in the
study projected a reduction in patient charges of $4.1 million per year.6
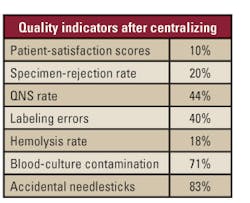
1. Quality indicators after centralizing phlebotomy at Sarah Bush
Lincoln Health Center, Matoon, IL.7
Reclaiming phlebotomy for the lab
Sarah Bush Lincoln Health Center (SBLHC) in
Matoon, IL, found a dramatic improvement on seven key quality benchmarks
after reclaiming phlebotomy for their laboratory (see Table 1).
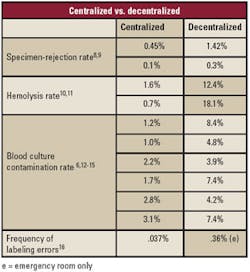
indicators in centralized vs. decentralized phlebotomy services.
“Decentralization creates a real disconnect
between the patient and the laboratory,” says Jodie Warner, MBA,
MT(ASCP) DLM, and director of Laboratory Services at SBLHC. “But what
really drove us back toward recentralizing our specimen-collection
services was the accidental needlestick rate.” According to Warner, the
facility's accidental needlestick rate declined 83% after recentralizing
phlebotomy. Many studies have been published comparing key quality
indicators in sample collection in centralized versus decentralized
environments (see Table 2). Indicators that show consistent improvement
by comparison in centralized settings include hemolysis,
specimen-rejection rates, blood-culture contamination, and mislabeled
samples.
But not every facility that decentralized has
returned to laboratory-based phlebotomy. St. John Hospital and Medical
Center in Detroit has been decentralized since 1996 and is likely to
remain that way for the near future.
“We estimate it will cost us $450,000 to
recentralize specimen collection back to the lab,” says Karla Bialk,
MSMT(ASCP), St. John's core laboratory director. “The nursing staff
cannot give up the 15 FTEs we will need to fill the phlebotomy positions
for recentralizing. So, if we are ever going to reclaim phlebotomy for
the laboratory, we have to find other ways to demonstrate the cost
savings to our administrators.” Bialk is hoping that by monetizing the
cost of rejected samples, mislabeled specimens, and the decreased
productivity, it will provide the necessary justification.
Denise Danko, MT(ASCP), St. John's operations
coordinator for phlebotomy, says the general consensus among the lab and
nursing departments is that phlebotomy should be recentralized, but
budget cuts and declining reimbursements are keeping it off the table —
at least for now. She asserts the staffing strategy is not
perfect, but it is functioning. “We currently have about 350 PCTs
drawing our patients' blood samples. It is not a perfect system, but one
of the reasons it has functioned this long is because the lab subjects
the PCTs to a comprehensive training class, 25 mandatory successful
venipunctures before drawing unsupervised, and, until recently, annual
competency assessments.” Danko says that St. John's nursing education
department dropped the phlebotomy assessments of their PCTs five years
ago due to lack of resources and the belief that all the effort the
organization had spent on the process was not impacting its Press-Ganey
patient-satisfaction scores.
Decentralized phlebotomy may not yet have run its
course, but many facilities conclude it should be a road less traveled.
With as many hazards and potholes today as when it was first conceived,
some get off at the first exit while others choose — or are told by
their administrators — to ride it out. This much is certain: 20-some
years after a certain author proclaimed the staffing strategy would
bring about the extinction of laboratory-based phlebotomists, their
preanalytical expertise is valued more now than ever. Instead of
threatening their future, decentralized phlebotomy is securing it.
Now, may I have the ketchup?
Dennis J. Ernst, MT(ASCP), is the director of the
Center for Phlebotomy Education in Corydon, IN, member of MLO's
“Tips from the Clinical Experts” panel, an MLO editorial advisory
board member, and editor of Phlebotomy Today. He can be contacted
through
www.phlebotomy.com .
References
- Ernst D. Is the phlebotomist obsolete? MLO.
1997;29(10);30-34. - Ernst D. Phlebotomy in 2010: a procedure, not a profession.
Lab Med. 1996;27(10):669. - Phlebotomy gets heightened attention for patient satisfaction.
The Dark Report. 2007;14(15):10-14. - Nelson K. Recentralizing phlebotomy services in the clinical
lab. Adv Med Lab Pro. 2002;14(22):21-24. - Zwang O, Albert R. Analysis of strategies to improve cost
effectiveness of blood cultures. J Hosp Med.
2006;1(5):272-276. - Gander R, Byrd L, DeCrescenzo M, Hirany S, Bowen M, Baughman J.
Impact of blood cultures drawn by phlebotomy on contamination rates
and health care costs in a hospital emergency department. J Clin
Microbiol. 2009;47(4):1021-1024. - Warner J. Phlebotomy Recentralization. Paper presented at: CLMA
ThinkLab '05; March 7, 2005, Chicago, IL. - Mannion H, Nadder, T. Three alternative structural
configurations for phlebotomy: a comparison of effectiveness.
Clin Lab Sci. 2007;20(4):210-214. - Southwick K. Back to the drawing board: hospitals rethink their
phlebotomy staffing practices. CAP Today. 2001:15(2)12-18. - Burns E, Yoshikawa N. Hemolysis in serum samples drawn by
emergency department personnel versus laboratory phlebotomists.
Lab Med. 2002;5(33):378-380. - Pretlow L, Gandy T, Kenimer-Leiback E, Russell B, Kraj B. A
quality improvement cycle: hemolyzed specimens in the emergency
department. Clin Lab Sci. 2008;21(4):219-224. - Weinbaum FI, Lavie S, Danek M, Sixsmith D, Heinrich G, Mills S.
Doing it right the first time. Quality improvement and the
contaminant blood culture. J Clin Micro. 1997;35(9):563-565. - Schifman R, Strand C, Meier F, Howanitz P. Blood culture
contamination. Arch Pathol Lab Med. 1998; 122: 216-220. - Warner JL. Recentralizing phlebotomy back into the laboratory.
Clin Leadersh Manag Rev. 2005 Jul 26;19(4):E3. - Bekeris LG, Tworek JA, Walsh MK, Valenstein PN. Trends in blood
culture contamination: a College of American Pathologists Q-Tracks
study of 356 institutions. Arch Pathol Lab Med. 2005
Oct;129(10):1222-1225. - Sandhaus L, Sauder K, Michelson E. Relative frequency of
mislabeled laboratory samples from the emergency department (ED)
compared to other hospital areas. Institute for Quality in Lab
Medicine (IQLM), 2005 IQLM Conference Poster Session.
http://cdc.confex.com/cdc/qlm2005/techprogram/paper_8547.htm .
Accessed October 26, 2009.