Diabetes cases continue to rise from SARS-CoV-2 complications
According to a number of studies regarding the effect of SARS-CoV-2 and diabetes, data shows that people with diabetes are not more prone to SARS-CoV-2, the virus that causes COVID infections, but if they develop an infection, the disease is much more severe and seems to progress quicker.
In addition, SARS-CoV-2 infections are associated with the worsening of diabetes symptoms, and persons with diabetes are at increased risk for severe COVID-19. SARS-CoV-2 infection might also induce newly diagnosed diabetes, according to a report from the Centers for Disease Control and Prevention (CDC).
According to a report from Mayo Clinic, people with diabetes have more inflammation in their body. Therefore, with COVID, that inflammatory state gets worse much more quickly. People with diabetes also may be more prone to having problems with their circulatory systems. It also appears to happen with both type 1 and type 2 diabetes, and both seem to be prone to more severe disease. However, Type 1 patients may have better outcomes because they are younger.1
Risk of diabetes after COVID
In the report from the CDC, Risk for Newly Diagnosed Diabetes >30 Days After SARS-CoV-2 Infection Among Persons Aged <18 Years — United States, March 1, 2020–June 28, 2021 ,2 published in January 2022, persons aged less than 18 years with COVID-19, were 116%, according to data from IQVIA (a database of adjudicated healthcare claims from closed U.S. health plans used to provide a complete view of patient care across all care setting), more likely to receive a new diabetes diagnosis 30 days after infection than were those without COVID-19 and those with pre-pandemic acute respiratory infections. The report also indicated that non-COVID respiratory infections were not associated with an increased risk for diabetes.The observed association between diabetes and COVID-19 might be attributed to the effects of SARS-CoV-2 infection on organ systems involved in diabetes risk. COVID-19 might lead to diabetes through direct attack of pancreatic cells expressing angiotensin converting enzyme 2 receptors; through stress hyperglycemia resulting from the cytokine storm and alterations in glucose metabolism caused by infection; or through precipitation of prediabetes to diabetes.10
A percentage of these new diabetes cases likely occurred in persons with prediabetes, which occurs in one in five adolescents in the United States. Steroid treatment during hospitalization might lead to transient hyperglycemia; however, only 1.5% – 2.2% of diabetes codes were for drug- or chemical-induced diabetes, with the majority of codes being for type 1 or type 2 diabetes.
Alternatively, COVID-19 might have indirectly increased diabetes risk through pandemic-associated increases in body mass index, a risk factor for both serious COVID-19 illness and diabetes. The authors commented that future studies addressing the role of comorbidities and increases in body mass index in post–COVID-19 diabetes are warranted.
Although this study provides information on the risk for diabetes following SARS-CoV-2 infection, additional data are needed to understand underlying pathogenic mechanisms, either those caused by SARS-CoV-2 infection itself or resulting from treatments, and whether a COVID-19–associated diabetes diagnosis is transient or leads to a chronic condition.Increases in pediatric type 1 diabetes
Evidence of increased pediatric type 1 diabetes has been reported during the COVID-19 pandemic.3,4 Among persons aged <18 years with COVID-19 and new diabetes diagnoses in this study, nearly one half had diabetic ketoacidosis (DKA) at or around the time of diagnosis. This number was higher than that in comparison groups, and higher than previous reports of DKA among incident type 1 diabetes cases before the pandemic (28%) .11 Increased frequency of DKA at time of diagnosis of type 1 diabetes during the pandemic has previously been reported and was thought to be due to delayed care-seeking for diabetes.5 However, the observed association of increased risk for diabetes diagnosis following SARS-CoV-2 infection would not be explained solely by delayed care. COVID-19 has disproportionately affected racial/ethnic minority groups, and those aged <18 years in these groups are also at increased risk for type 2 diabetes.12An association between COVID-19 and new pediatric diabetes diagnoses might disproportionately affect racial/ethnic minority groups. Race/ethnicity data were unavailable in the present data sets; however, future studies should address racial and ethnic disparities in COVID-19 and diabetes, and whether persons aged <18 years who are at risk for COVID-19 are also those at risk for delaying medical care.
Healthcare providers should screen for diabetes symptoms in persons aged < 18 years with a history of SARS-CoV-2 infection. These symptoms can include frequent urination, increased thirst, increased hunger, weight loss, tiredness or fatigue, stomach pain, and nausea or vomiting.
The stats
The increased diabetes risk among persons aged <18 years following COVID-19, highlights the importance of COVID-19 prevention strategies in this age group, including vaccination for all eligible persons and chronic disease prevention and treatment.
The COVID-19 pandemic has disproportionately affected people with diabetes, who are at increased risk of severe COVID-19. Increases in the number of type 1 diabetes diagnoses and increased frequency and severity of DKA at the time of diabetes diagnosis have been reported in European pediatric populations during the COVID-19 pandemic.
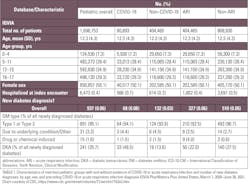
The study included 80,893 patients with COVID-19 in the IQVIA database, the mean age was 12.3 years, 50.1% were female, and 0.7% were hospitalized at their index COVID-19 encounter. In the IQVIA database, diabetes incidence was 316 per 100,000 person-years in the COVID-19 group, 118 per 100,000 person-years in the pandemic period non–COVID-19 group, 126 per 100,000 person-years in the pre-pandemic acute respiratory infection group (ARI), and 125 per 100,000 person-years in the pre-pandemic non-ARI group.
References
Barrett CE, Koyama AK, Alvarez P, et al. Risk for Newly Diagnosed Diabetes >30 Days After SARS-CoV-2 Infection Among Persons Aged <18 Years — United States, March 1, 2020–June 28, 2021. MMWR Morb Mortal Wkly Rep 2022;71:59–65. DOI: http://dx.doi.org/10.15585/mmwr.mm7102e2 https://www.cdc.gov/mmwr/volumes/71/wr/mm7102e2.htm#Kristine Russell