AI blood testing technology can detect lung cancers
The test approach, called DELFI (DNA evaluation of fragments for early interception), spots unique patterns in the fragmentation of DNA shed from cancer cells circulating in the bloodstream. Applying this technology to blood samples taken from 796 individuals in Denmark, the Netherlands and the U.S., investigators found that the DELFI approach accurately distinguished between patients with and without lung cancer.
Combining the test with analysis of clinical risk factors, a protein biomarker, and followed by computed tomography imaging, DELFI helped detect 94% of patients with cancer across stages and subtypes. This included 91% of patients with earlier or less invasive stage I/II cancers and 96% of patients with more advanced stage III/IV cancers.
The DELFI technology uses a blood test to indirectly measure the way DNA is packaged inside the nucleus of a cell by studying the size and amount of cell-free DNA present in the circulation from different regions across the genome. Healthy cells package DNA like a well-organized suitcase, in which different regions of the genome are placed carefully in various compartments. The nuclei of cancer cells, by contrast, are like more disorganized suitcases, with items from across the genome thrown in haphazardly. When cancer cells die, they release DNA in a chaotic manner into the bloodstream.
DELFI helps identify the presence of cancer using machine learning, a type of artificial intelligence, to examine millions of cell-free DNA fragments for abnormal patterns, including the size and amount of DNA in different genomic regions. This approach provides a view of cell-free DNA referred to as the “fragmentome.” The DELFI approach only requires low coverage sequencing of the genome, enabling this technology to be cost-effective in a screening setting.
The DELFI approach found that patients who were later determined to have cancer had widespread variation in their fragmentome profiles, while patients found not to have cancer had consistent fragmentome profiles.
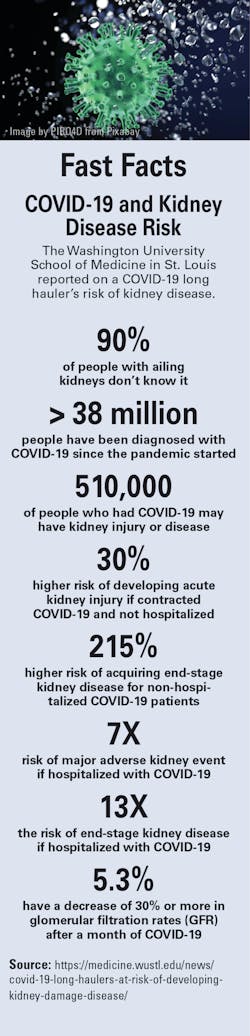
High virus count in the lungs drives COVID-19 deaths
The buildup of coronavirus in the lungs is likely behind the steep mortality rates seen in the pandemic, a study finds. The results contrast with previous suspicions that simultaneous infections played major roles in heightened risk of death, according to a news release from NYU Langone Health.
Led by researchers at NYU Grossman School of Medicine, the study shows that people who died of COVID-19 averaged 10 times the viral load in their lower airways as did severely ill patients who survived their illness. Investigators found no evidence implicating a secondary bacterial infection as the cause of the deaths, but they cautioned this may from frequent antibiotics given to critically ill patients.
Current guidelines from the Centers for Disease Control and Prevention (CDC) do not encourage the use of antivirals, such as remdesivir, for severely ill patients on mechanical ventilation. The NYU Langone study results suggest that these medications may still yet remain a valuable tool in treating these patients, though more researcher may be needed.
Despite previous concerns that the virus may prompt the immune system to attack the body’s own lung tissue and lead to dangerous levels of inflammation, the investigators found no evidence that this was a major contributor to COVID-19 deaths in the group studied. In fact, researchers said that the strength of the immune response appeared proportionate to the amount of virus in the lungs.
COVID-19 patients placed on mechanical ventilators in order to breathe fare particularly poorly, with 70 percent nationwide succumbing to the illness. Notably, experts attribute the high mortality seen in other viral pandemics such as the Spanish flu in 1918 and swine flu in 2009 to a secondary bacterial infection. However, it remained unclear whether a similar issue affected people with COVID-19.
The study, recently published in Nature Microbiology, was to clarify the role of secondary infections, viral load, and immune cell populations in COVID-19 mortality.
However, the investigators only studied patients with coronavirus who survived their first two weeks of hospitalization. It is possible that bacterial infections or autoimmune reactions may play a greater role in COVID-19 mortality that occurs earlier.
NIH study shows no benefit from convalescent plasma for some COVID-19 outpatients
The final results of the Clinical Trial of COVID-19 Convalescent Plasma in Outpatients (C3PO) demonstrate that COVID-19 convalescent plasma did not prevent disease progression in a high-risk group of outpatients with COVID-19 when administered within the first week of their symptoms.
The trial was stopped in February 2021 due to lack of efficacy based on a planned interim analysis. The formal conclusions from the trial, which was funded primarily by the National Heart, Lung, and Blood Institute (NHLBI), part of the National Institutes of Health, and by the Biomedical Advanced Research and Development Authority (BARDA), part of the Office of the Assistant Secretary for Preparedness and Response at the U.S. Department of Health and Human Services, appear in the New England Journal of Medicine.
“We were hoping that the use of COVID-19 convalescent plasma would achieve at least a 10% reduction in disease progression in this group, but instead the reduction we observed was less than 2%,” said Clifton Callaway, MD, PhD, the contact principal investigator for the C3PO trial and Professor of Emergency Medicine at the University of Pittsburgh.
Last year, the U.S. Food and Drug Administration (FDA) issued an emergency use authorization (EUA) to allow use of convalescent plasma in hospitalized patients with COVID-19. Researchers wanted to know whether administering COVID-19 convalescent plasma might also be beneficial in persons who were recently infected with SARS-CoV-2, the virus that causes the disease, but who were not severely ill and could be treated as outpatients. The objective was to prevent progression to severe COVID-19 illness.
The randomized, controlled clinical trial involved adult outpatients who presented to emergency departments with mild COVID-19 symptoms during their first week post-infection and had at least one risk factor for progression to severe COVID-19, such as obesity, hypertension, diabetes, heart disease, or chronic lung disease. They were randomly assigned to receive treatment with either high-titer COVID-19 convalescent plasma (containing anti-COVID-19 antibodies) or placebo (salt solution infused with multivitamins and lacking antibodies). The researchers found no significant difference in disease progression between the two groups.
CDC study finds unvaccinated people nearly 5 times more likely to get COVID-19
People who are not vaccinated against COVID-19 are 4.9 times more likely to get COVID-19 and the 29.2 times more likely to be hospitalized than fully vaccinated people, the Centers for Disease Control and Prevention (CDC) reported in its Morbidity and Mortality Weekly Report (MMWR). That was based on data from Los Angeles County on July 25, when the Delta variant was pervasive.
Among 43,127 reported SARS-CoV-2 infections in residents at least 16 years of age, 10,895 (25.3%) were in fully vaccinated people, 1,431 (3.3%) were in partially vaccinated people, and 30,801 (71.4%) were in unvaccinated people.
Fewer fully vaccinated people infected with SARS-CoV-2 were hospitalized (3.2%), admitted to an intensive care unit (0.5%), and required mechanical ventilation (0.2%), compared with partially vaccinated people (6.2%, 1.0%, and 0.3%), and unvaccinated people (7.6%, 1.5%, and 0.5%).
During May 1-July 25, the percentages of B.1.617.2 (Delta) variant infections estimated from 6,752 samples with lineage data increased among fully vaccinated persons (from 8.6% to 91.2%), partially vaccinated persons (from 0% to 88.1%), and unvaccinated persons (from 8.2% to 87.1%).
Whole genome sequencing (WGS)-based SARS-CoV-2 lineages and cycle threshold (Ct) values from qualitative reverse transcription-polymerase chain reaction (RT-PCR) for two SARS-CoV-2 gene targets, including the nucleocapsid (N) protein gene region and the open reading frame 1 ab (ORF1ab) polyprotein gene region, were reported for a sample of the specimens.
CDC and FDA collaborate on Antibiotic Resistance Isolate Bank
The U.S. Food and Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC) have teamed up to create a repository of resistant bacterial and yeast isolates of national medical concern that have been phenotypically and genotypically characterized.
Called the Antibiotic Resistance Isolate Bank (AR Isolate Bank), it contains isolate panels that are available free of charge as a resource for developing drugs and diagnostic testing panels.
Routinely updated, the AR Isolate Bank has new resistant isolates and their corresponding resistance markers. The isolates are preassembled into panels and upon request, isolates and/or panels are shipped to diagnostic and pharmaceutical companies, academia, as well as clinical and public health laboratories. For example, academic medical centers or private and reference laboratories may use the panels and isolates to create lab developed tests (LDTs).
As of February 2021, the bank had 29 panels and 952 isolates.
Available panels and ordering instructions can be found on the AR Isolate Bank on CDC.gov and can be used in development of diagnostic tests and in studies; however, the FDA will also accept premarket submissions that use well-characterized isolates from other sources. The isolates in the AR Isolate Bank may be helpful in challenging tests for the detection of infectious diseases and their associated resistance mechanisms, as well as antimicrobial susceptibility testing devices, to ensure the tests can efficiently detect a variety of resistant microorganisms and/or molecular markers of resistance.
Derived from various specimen sources and emerging resistance mechanisms, the isolates in the AR Isolate Bank are from healthcare-associated and community-associated infections, foodborne illnesses, and sexually transmitted infections, such as gonorrhea. Each isolate is verified for purity and identified using matrix-assisted laser desorption-ionization time of flight mass spectrometry (MALDI-TOF MS) and 16S rRNA gene sequencing (as needed). Antimicrobial susceptibility testing (AST) is performed using the reference broth microdilution method in accordance with Clinical and Laboratory Standards Institute (CLSI) standards. In addition, whole genome sequencing is performed on isolates to identify resistance markers and to better understand the genotypic basis of resistance.