Benefits of high-dose blood thinners in COVID-19 patients unclear
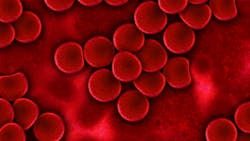
While COVID-19 infected patients should be treated with standard anticoagulation therapies, such as blood thinning medication, a new study by researchers at the George Washington University (GW) suggests that anticoagulating patients at higher doses, without traditional medical indications to do so, may be ineffective and even harmful, according to a press release.
The study was published in the journal Thrombosis Research.
The research team evaluated 402 patients diagnosed with COVID-19 admitted to GW Hospital between March 15 and May 31, 2020. Clinical outcomes were compared between 152 patients treated with high-dose blood thinners, and 250 patients treated with the standard low-dose blood thinners, typically prescribed to hospitalized medical patients.
“While it’s true that COVID-19 patients could be dying of blood clots, the data we’ve evaluated does not support giving every patient a high dose of blood thinners. That’s a challenge, as the benefits still remain unclear,” said Lei Lynn, MD, first author of the study and Assistant Professor of Medicine at GW SMHS. “We caution against an aggressive blood thinner regimen for everyone, unless there is clear evidence to do so.”
At the beginning of the pandemic, all patients admitted with COVID-19 to the GW Hospital were treated with standard dose anticoagulation, unless contraindicated. As awareness of the elevated risk of blood clots developed, many providers began treating patients with high-dose blood thinners. At GW Hospital, for non-critically ill patients, medical teams were advised to especially consider initiating a high dose of anticoagulation if a patient’s D-dimer level exceeded 3 micrograms per milliliter. The research team previously published a study finding higher levels of the biomarker D-dimer, a medical indicator found in the blood, is associated with higher odds of clinical deterioration and death from COVID-19.