People with cancer sickened by COVID-19 have a crude death rate of 13 percent, according to the largest series of data released thus far from a multinational perspective. The data on more than 900 patients, published in The Lancet and simultaneously presented at ASCO20 Virtual, also revealed cancer-specific factors associated with increased mortality.
The information is the first report from an ongoing international initiative by the COVID-19 and Cancer Consortium (CCC19) to track outcomes within this vulnerable population. The CCC19 registry was built and is maintained as an electronic REDCap database housed at Vanderbilt University Medical Center. The data in this first report from CCC19 was gathered from 928 patients in Spain, Canada and the United States.
“While older patients and those with major comorbid conditions are at substantially increased risk of dying from COVID-19, our early findings are encouraging news for patients without major medical conditions who receive their cancer therapy within four weeks of their infection. However, more data are needed to reliably assess individual higher risk therapies,” said Nicole Kuderer, MD, with the Advanced Cancer Research Group in Seattle, one of the study’s lead authors.
These early data showed no statistical association between 30-day mortality and cancer treatments, suggesting that surgery, adjuvant chemotherapy and maintenance chemotherapy could continue during the pandemic with “extreme caution.”
The cancer-specific factors associated with increased mortality included having an Eastern Cooperative Oncology Group (ECOG) performance status of two or worse. ECOG is a grading scale for measuring how cancer impacts a patient’s daily living abilities. A score of two designates a patient who is capable of self-care but unable to work and who is up and about more than 50 percent during waking hours. Another factor associated with increased mortality was an active cancer status, particularly progressive cancer.
The mortality risk also increased with the number of comorbidities, such as hypertension or diabetes, particularly with two or more comorbidities. As is the case with the non-cancer population, mortality increased with age. Mortality was 6 percent for cancer patients younger than 65, 11 percent for those 65-74 and 25 percent for those older than 75. Males also had a higher death rate than females, 17 percent compared to 9 percent.
CCC19 was formed to rapidly collect data as part of an effort to understand the unique effects the coronavirus has on people with cancer.
Study: Remdesivir benefits some COVID-19 patients
A study published in the New England Journal of Medicine found that hospitalized COVID-19 patients who received Gilead Sciences’ antiviral drug remdesivir recovered a median of four days earlier than those who received a placebo.
Preliminary findings from the double-blind Adaptive COVID-19 Treatment Trial (ACTT-1), sponsored by the U.S. National Institute of Allergy and Infectious Diseases (NIAID), showed that 538 patients randomly assigned to receive remdesivir had a median recovery time of 11 days, compared with 15 days in the 521 patients who received a placebo.
The patients were enrolled from February 21 to April 19 at 60 study sites and 13 subsites in the United States and Mexico (79.8 percent), Europe (15.3 percent), and Asia (4.9 percent), on the basis of the evolving epidemiology of the pandemic. Patients received either a placebo for 10 days or remdesivir intravenously as a 200-milligram (mg) loading dose followed by 100-mg maintenance doses for the next nine days or until release from the hospital or death. The analysis includes only patients with at least some post-baseline data available.
The most common disease severity score, rated from 1 (not requiring hospitalization) to 8 (dead), was 5 (needing oxygen). In patients with a score of 5, remdesivir was associated with a 47 percent speedier recovery, versus 20 percent in patients with a score of 6 (needing high-flow ventilation), and only 0.05 percent in patients with a score of 7 (needing intubation or extracorporeal membrane oxygenation [oxygen added to the blood outside the body]).
The authors noted that patients requiring supplemental oxygen derived the most benefit from remdesivir, while it did not benefit those requiring more intense treatments. After the NIAID made the results public late last month, the U.S. Food and Drug Administration on May 1 issued an emergency use authorization (EUA) for remdesivir for the treatment of seriously ill COVID-19 patients. The authors also suggested further study to evaluate outcomes from antivirals combined with other therapeutic agents.
No improvement in death rate for COVID-19 patients who received hydroxychloroquine
A research team led by investigators from Brigham and Women’s Hospital has evaluated real-world evidence related to outcomes for COVID-19 patients who were treated with hydroxychloroquine or chloroquine analogues (with or without a macrolide). Investigators found no evidence that either drug regimen reduced the death rate among patients. Patients treated with hydroxychloroquine or chloroquine regimens were far more likely to experience abnormal, rapid heart rhythms (known as ventricular arrhythmias) than their counterparts who had not received the drugs. The team’s findings are published in The Lancet.
“No matter which way you examine the data, use of these drug regimens did not help,” said corresponding author Mandeep R. Mehra, MD, executive director of the Brigham’s Center for Advanced Heart Disease. “If anything, patients had a higher likelihood of death. We also saw a quadrupling in the rate of significant ventricular arrhythmias in patients with COVID-19 who had been treated with hydroxychloroquine or chloroquine regimens.”
Mehra and colleagues conducted their study using the Surgical Outcomes Collaborative database, an international registry comprised of de-identified data from 671 hospitals across six continents. The analysis included data on more than 96,000 patients hospitalized with COVID-19. This included almost 15,000 patients who had received the anti-malarial drug chloroquine or its analog hydroxyquinone with or without an antibiotic (macrolides such as azithromycin and clarithromycin) early after COVID-19 diagnosis. The study’s primary endpoint was death or discharge from the hospital.
Mehra and colleagues found that 10,698 patients died in the hospital (11.1 percent) and 85,334 survived to discharge. The team compared death rates for those taking one of the drug regimens to that of a control group, after accounting for confounding variables, such as age, sex, and underlying risk factors. The death rate among the control group was 9.3 percent. Each of the drug regimens of chloroquine or hydroxychloroquine alone, or in combination with a macrolide, was associated with an increased risk of in-hospital death with COVID-19.
In addition, each of the drug regimens was associated with an increase in the risk of ventricular arrhythmia. Among the treatment groups, between 4 and 8 percent of patients experienced a new ventricular arrhythmia, compared to 0.3 percent of patients in the control group.
Chloroquine and hydroxychloroquine have been known to cause cardiovascular toxicity and previous studies have shown that macrolides can increase the risk of sudden cardiac death. A preliminary analysis of patients in Brazil treated with chloroquine and an antibiotic has suggested a high dose of chloroquine may be a safety hazard. Results from randomized, controlled clinical trials are not expected until the summer.
The authors caution that the current study is observational in nature – this means that it cannot absolutely answer the question of whether the drug regimens were solely responsible for the changes in survival. Randomized clinical trials will be required before any conclusion can be reached regarding harm.
“These findings suggest that these drug regimens should not be used outside of the realm of clinical trials and urgent confirmation from randomized clinical trials is needed,” the authors conclude.
NIH launches study to investigate pregnancy outcomes resulting from COVID-19
The National Institutes of Health (NIH) has launched a multipronged study to understand the effects of the COVID-19 pandemic during and after pregnancy. Researchers will analyze the medical records of up to 21,000 women to evaluate whether changes to healthcare delivery that were implemented as a result of the pandemic have led to higher rates of pregnancy-related complications and cesarean delivery. They also seek to establish the risk of pregnant women with COVID-19 infection transmitting the virus to their fetus. Newborns will be monitored and assessed until they are discharged from the hospital.
In addition, the study will track more than 1,500 pregnant women confirmed with COVID-19 infection, monitoring their health for six weeks after childbirth.
The study will be conducted by researchers in the Maternal-Fetal Medicine Units (MFMU) Network, a group of 12 U.S. clinical centers funded by NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). MFMU Network sites cover more than 160,000 deliveries a year, and their racial, ethnic, and geographic diversity allows researchers to generalize their study findings to the U.S. population.
MFMU Network investigators plan to contribute data collected from the current study to a larger registry to help inform future studies of how COVID-19 affects maternal health and pregnancy.
No benefit of convalescent plasma in COVID-19 patients, study finds
Convalescent plasma therapy did not help 52 seriously ill COVID-19 patients recover in the first known randomized study of its kind, although it was stopped early because of low enrollment. The study, published in JAMA, involved coronavirus patients with severe illness (respiratory distress and/or low oxygen levels) or life-threatening disease (shock, organ failure, or the need for mechanical ventilation) in seven medical centers in Wuhan, China, from February 14 to April 1, with final follow-up on April 28.
The trial was stopped early because, owing to containment of the Wuhan outbreak, researchers were able to recruit only 103 of 200 patients needed to generate a clinically meaningful result. One patient withdrew from the study, and one in the control group received convalescent plasma, a protocol violation, because of a life-threatening infection.
Convalescent plasma therapy, which dates back to the early 20th century, involves the transfusion of blood plasma collected from patients recovered from infection to improve immune response in the recipient. Although evidence supporting its use in COVID-19 patients is scarce, the U.S. Food and Drug Administration (FDA) recently approved its emergency use in patients who have severe or life-threatening coronavirus infection.
The authors noted that most previous studies on convalescent plasma lacked standardization and procedure control in donor selection and the type or level of antibodies in the convalescent plasma. The researchers called for further studies on optimal patient selection and timing of convalescent plasma therapy in COVID-19 patients.
In a commentary in the same journal, Arturo Casadevall, MD, PhD, of the Johns Hopkins Bloomberg School of Public Health in Baltimore and colleagues said that while convalescent plasma didn’t lead to significant improvements in clinical status or death rate, the study generated “potentially hopeful signals,” adding that convalescent plasma may be useful in combination with antiviral drugs.
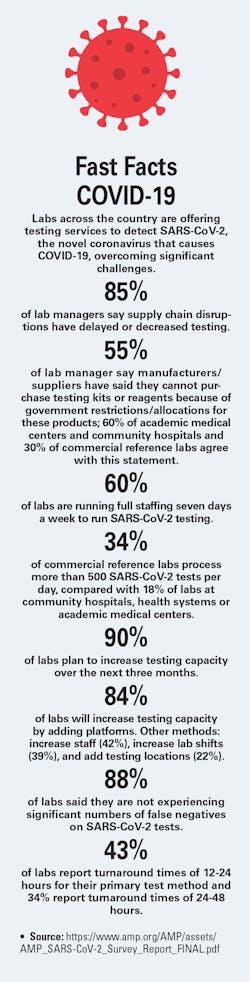
Source: https://www.amp.org/AMP/assets/AMP_SARS-CoV-2_Survey_Report_FINAL.pdf