The difficulty of predicting seasonal flu outbreak severity and associated testing demand can present a formidable challenge for clinical laboratories. But the lack of an effective plan to manage heavy flu testing demand can have significant ramifications for entire healthcare systems. They may include increased staff workloads and elevated stress levels, strained resources, overcrowding in patient care settings, and delays in time to diagnosis—which can cause associated delays in appropriate patient isolation measures and, potentially, inappropriate or delayed therapeutic interventions. Laboratorians who want to reevaluate their current flu testing protocols now have access to new predictive tools and a broader range of CLIA-waived testing options that can improve diagnostic accuracy at the point of care (POC).
Forecasting and nowcasting
Together with traditional influenza forecasting, the use of real-time data and machine learning—or “nowcasting”—has become a valuable tool to assist labs in preparing for flu season and making ongoing modifications to testing protocols throughout the season based on emerging trends.
The CDC collects data from both public health and clinical labs regarding the total number of respiratory specimens tested for influenza and the number of specimens that test positive for influenza by virus type. This data is used to produce a weekly surveillance report known as FluView,3 which informs labs about the presence and spread of influenza viruses in their geographic areas and helps them anticipate demand for testing. However, there is a slight lag between the weekly reports and actual influenza activity.
To address this issue, research teams have devised methods to estimate influenza-like illness in near-real time. The new methods take advantage of the large volume of diagnostic and syndromic data being reported from healthcare and public health settings to aid with infectious disease control efforts and decisions through the use of models. The methods incorporate a variety of techniques, from statistical modeling and machine learning to mechanistic and epidemiological models. Many utilize web-based data sources such as Internet search frequencies and electronic health records (EHRs),4 and they generate outputs such as influenza epidemic detection, peak timing prediction, and peak intensity prediction.5
Optimizing testing protocols
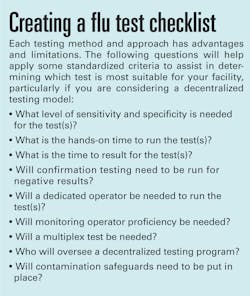
Developing an optimal flu readiness plan involves more than allocating staff and stocking a sufficient number of tests to meet anticipated demand. There are several factors lab and healthcare networks should consider in order to develop a flu readiness plan that is cost-effective and matches up well with the institution’s workflow capabilities and testing protocols.
Test sensitivity and specificity. For an illness with a 48-hour effective therapeutic window, like influenza, the ability to accurately detect and identify the pathogen is clearly of critical importance in diagnostic testing. In the categories of sensitivity and specificity, viral culture and nucleic acid amplification testing (NAAT) provide the best performance.6 While antigen-based Rapid Influenza Diagnostic Tests (RIDTs) have been widely used, their relatively low sensitivity (about 50 percent in some studies) compelled the FDA in 2017 to reclassify them from Class I to Class II devices with special controls.7 The agency put the special controls in place for RIDT manufacturers to increase sensitivity and undergo annual strain testing.8 The higher sensitivity and specificity of NAAT, which is now available in CLIA-waived settings for flu testing, can also eliminate the need for laboratory confirmation of negative results. In addition, recently updated clinical practice guidelines from the Infectious Diseases Society of America (IDSA) recommend the use of rapid molecular assays over RIDTs or antigen-based tests in outpatient settings to improve detection of influenza virus infection.9
Turnaround time. Because of their high sensitivity, viral culture and lab-based polymerase chain reaction (PCR) testing are often used in tandem to determine circulating influenza strains and define subtypes. However, normal turnaround time (TAT) for these lab-based tests is 48 hours or more. Because antiviral therapies must typically be initiated within 48 hours of onset of clinical symptoms for the patient to receive optimal benefit, labs need to deliver a faster time to result. One way to achieve this without sacrificing sensitivity and specificity is to deploy CLIA-waived molecular testing (NAAT) at the POC. Several studies demonstrate that timely influenza diagnosis may decrease unnecessary laboratory testing for other etiologies, support antiviral and antibiotic stewardship, and improve the effectiveness of infection prevention and control measures.10,11
Workflow and staffing. Testing methods and sites (e.g., central lab vs. POC) can vary considerably in their impact on workflow and what staff resources are required. For example, with the implementation or expansion of point-of-care testing (POCT), labs may need to consider location-specific staffing needs and hands-on time required to meet the demands of increased patient traffic during periods of high influenza activity. The hands-on time is an especially important factor to consider if a test itself has a fast TAT but running the test requires a lengthy set-up process or is labor-intensive for the operator. The workflow time allowance can be significantly greater if a method is used that requires confirmation testing for negative results, such as RIDTs.
Multiplex testing. Some test methods incorporate multiplex assays, or combination tests, which detect multiple pathogens in a single test. For example, there is an overlap in the clinical symptoms and seasonality of influenza and respiratory syncytial virus (RSV). The use of a multiplex molecular test that simultaneously detects influenza types A and B and RSV simplifies the test protocol, reduces diagnostic uncertainty, and helps guide treatment decisions. Also, the prompt, accurate detection of influenza and RSV infections can help quickly identify local outbreaks of disease.12
Cost. While both RIDTs and some NAATs are CLIA-waived for use in POC settings, the molecular tests are typically more expensive on a cost-per-test basis. However, the cost differential can be much smaller or even reversed when the overall clinical impact is included in the analysis. One study, for example, indicated significant cost savings for an institution’s flu testing program through NAAT implementation in the emergency department setting.13 To be accurate, cost analyses should take into account the potential clinical and workflow impact of the implementation of a test method in a decentralized setting across an entire institution.
Contamination concerns. Despite the advantages associated with establishing CLIA-waived molecular testing in a decentralized model, it’s important to note that any NAAT platform deployed at the POC should have a safeguard in place, such as a closed system design, to offer protection from possible environmental nucleic acid contamination. One study purposefully contaminated a CLIA-waived NAAT system and still found that, despite contamination, all negative results were reported negative. However, with any molecular testing, reducing the risk of contamination is an important consideration.14
Conclusion
Staying aware of real-time influenza trends as they emerge, and evaluating your current testing protocols through a new lens can help you prepare an optimal flu readiness plan for your health system and help your lab navigate the challenges of the upcoming flu season.
REFERENCES
- Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD). 2018-2019 U.S. Flu Season: Preliminary Burden Estimates. (May 2019) Retrieved from https://www.cdc.gov/flu/about/burden/preliminary-in-season-estimates.htm July 2019.
- Centers for Disease Control and Prevention, NCIRD. Vaccine Effectiveness: How Well Do the Flu Vaccines Work? Questions & Answers. (October 2018) Retrieved from https://www.cdc.gov/flu/vaccines-work/vaccineeffect.htm July 2019.
- Centers for Disease Control and Prevention, NCIRD. Weekly U.S. Influenza Surveillance Report. (July 5, 2019) Retrieved from https://www.cdc.gov/flu/weekly/index.htm July 2019.
- Lu FS et al. Improved state-level influenza nowcasting in the United States leveraging Internet-based data and network approaches. Nature Communications. 2019; 10:147.
- Spreco A et al. Integrated Detection and Prediction of Influenza Activity for Real-Time Surveillance: Algorithm Design. J Med Internet Res. 2017 June;19(6):e211
- Merckx J et al. Diagnostic Accuracy of Novel and Traditional Rapid Tests for Influenza Infection Compared With Reverse Transcriptase Polymerase Chain Reaction: A Systematic Review and Meta-analysis. Ann Intern Med. 2017 Sep 19;167(6):394-409.
- Green DA and St George K. Rapid Antigen Tests for Influenza: Rationale and Significance of the FDA Reclassification. J Clin Microbiol. 2018 Oct 56;10:e00711-18.
- FDA Reclassifies Influenza Test Systems as Class II. FDAnews Device Daily Bulletin. January 30, 2017.
- Uyeki TM et al. Clinical Practice Guidelines by the Infectious Diseases Society of America: 2018 Update on Diagnosis, Treatment, Chemoprophylaxis, and Institutional Outbreak Management of Seasonal Influenza. Clin Infect Dis. 2019 Mar 5;68(6):e1-e47.
- Dale AP et al. Impact of a Rapid Point of Care Test for Influenza on Guideline Consistent Care and Antibiotic Use. J Am Board Fam Med. 2019 Mar-Apr;32(2):226-233.
- Babady NE et al. CLIA-waived molecular influenza testing in the emergency department and outpatient settings. J Clin Virol. 2019 Jul;116:44-48.
- Drews SJ et al. What is the role of rapid molecular testing for seniors and other at-risk adults with respiratory syncytial virus infections? J Clin Virol. 2019 May;117:27-32.
- Hansen GT et al. Clinical decision making in the emergency department setting using rapid PCR: Results of the CLADE study group. J Clin Virol. 2018 May;102:42-49.
- Phillips JE et al. Assay Integrity of a PCR Influenza Point-of-Care Test Remains Following Artificial System Contamination. The Journal of Applied Laboratory Medicine. Jul 2019, jalm.2018.028639.
About the Author
Jamie E. Phillips, PhD
serves as Senior Scientific Affairs Manager, Point of Care, at Roche Diagnostics in Indianapolis, Indiana