It is estimated that nearly one in every 10 Americans is living with diabetes, with 1.5 million adults being newly diagnosed every year. Diabetes impacts over 30 million Americans and remains the 7th leading cause of death in the United States. Properly controlled diabetes can reduce mortality rates, yet nearly one third of Americans who have this condition remain undiagnosed.1 This means the reliable detection of diabetes through HbA1c testing can have life or death consequences for millions of Americans annually.
Because HbA1c tests can be performed easily without fasting or having to drink anything, this test is often the first indicator that diabetes is present for patients. For those already diagnosed, the test provides insight into how well the patient is adhering to their treatment plan, or how well the treatment plan itself is working. Although a diabetes diagnosis is decided by HbA1c levels of 6.5 percent or higher, this test is also an effective means for determining prediabetes in patients with ranges between 5.7 percent to 6.4 percent. In prediabetic patients, studies have shown that moderate exercise and losing 7 percent of one’s body weight can reduce a patient’s risk of type 2 diabetes by 58 percent.2
Impact of preanalytical errors
It has become standard practice to perform the HbA1c test using a point-of-care (POC) system with a capillary blood sample. Compared to venous blood draws, capillary blood sampling has the advantage of being easier and faster to perform. Yet, despite its simplicity, obtaining a quality capillary blood sample can pose challenges—and if done improperly, can contribute to preanalytical errors. With a pervasive and destructive disease such as diabetes, diagnostic errors can have dire consequences. Even failing to detect prediabetes does patients a disservice, because it deprives them of a chance to correct behaviors that could prevent a chronic, life-altering condition.
Fortunately, many capillary testing challenges are easily overcome by following best practices and industry guidelines. By ensuring tools and sampling are performed appropriately, higher success rates can be achieved.
Five tips for reducing preanalytical errors
1. Know your blood volume requirements
The volume of blood required to perform a diagnostic test varies depending on the POC device being used and the specific test being conducted. As newer technology has emerged, blood volume requirements have been greatly reduced. Different POC devices perform optimally with specific sample sizes and too little or too much blood can impact readings. Familiarizing yourself with the blood volume requirements for your POC device is an essential first step.
Blood volume requirements vary by the type of test being performed and the number of tests being performed. When run alone, HbA1c tests require very low blood volumes (1-5ul)3 that are typically achieved with thin lancets at shallow puncture depth (i.e., 30G x 1.5mm or 28G x 1.8mm). If performing multiple tests or testing on an individual with thicker skin, it may be necessary to use a larger lancet and puncture deeper.
2. Choose the right lancet
Safety lancets are available in a range of sizes and activation methods and determining which lancet to use will depend upon the patient, the diagnostic test for which the sample is required, and consideration of pain reduction. The latter factor is especially important for patients from whom samples must be collected repeatedly.
The World Health Organization (WHO) reports that pain increases with lancet penetration depth,4,5 which is partly determined by the length of the lancet being used. It notes that, when finger sampling in adult populations, the depth of penetration should not go beyond 2.2mm and that pressure applied during sampling compresses the skin so that ultimate puncture depth will be slightly greater than the length of lancet used.
In the U.S., many hospitals and labs carry specific lancet brands as per contractual arrangements, and often have several size variants available within the line(s) they carry. Safety lancet specifications vary by depth of penetration and gauge size. The depth of penetration is pre-set and straightforward, with some safety lancets going as deep as 3.0mm and others as shallow as 0.5mm. Assuming other variables are constant, the deeper the lancet penetrates, the greater the blood volume it will produce. Gauge size dictates the diameter of a lancet. Unlike depth of penetration, the higher the gauge size, the smaller the lancet diameter. For example, a 30-gauge lancet is thinner than an 18-gauge, and if all other variables are constant, should result in a smaller blood sample. Beyond device specifications, bevel geometry and activation method may also impact blood volume, and these will vary by manufacturer.
3. Selecting a suitable sample site
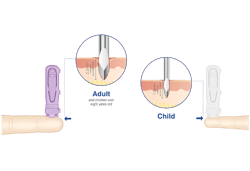
For adults and children over 6 months (weighing more than 22lbs), WHO recommends testing be done of the side of the ball of the finger and should be restricted to the middle and ring fingers. The thumb and index fingers are precluded because of the potential for calluses, and the little finger because the tissue is thin and there is a higher risk of hitting bone.4
There are a number of factors which influence the possible blood volume derived from any given sampling episode. These include patient hand temperature, lancet specification, and post-lancing massage technique. Research has highlighted the wide variation of blood volume achieved from site to site in the same patient and with the use of different post-lancing techniques, such as pressure application.6 When conducting a POC test, it is recommended that the safety lancet needle gauge (thickness) and length be chosen to collect the minimum volume of blood required to successfully complete the diagnostic test.
4. Perfecting your technique
Technique is important for reducing sample contaminants and for achieving adequate blood flow.
Prior to lancing, the sample site should be cleaned with alcohol and allowed to dry.4 If a large blood volume is required, the sample site can be warmed prior to cleaning. Ideally, the site should then be lanced in one quick motion, and the first drop of blood wiped away to avoid contaminating the sample with tissue fluid or debris. Gentle pressure should then be applied to encourage the flow of blood into the collection device, while avoiding pressing too vigorously, as this may dilute the sample with plasma and increase the probability of hemolysis.4
5. The patient’s experience
Research into the pain associated with the use of safety lancets highlights that the key factors implicated are ease of skin penetration and the size of the resultant injury.5 The first of these factors is determined by lancet geometry and the quality of the lancet tip. The second factor is determined by lancet diameter and penetration depth. In order to make the procedure as comfortable as possible for the patient, a good quality lancet should always be selected, with a lancet size that provides just enough blood for the procedure. Some safety lancets go further to help reduce pain, with design features that reduce pressure or help distract the nerve endings.
Conclusion
POC testing offers a fast and reliable means for conducting HbA1c testing, however it may be subject to preanalytical errors if capillary sampling is not performed appropriately. By understanding blood volume requirements, selecting the right tools, and following best practices it may be possible to reduce preanalytical errors for improved testing accuracy. With HbA1c representing a key means of identifying diabetes and prediabetes, as well as treatment efficacy over time, accurate results are imperative to helping improve outcomes for millions of patients living with diabetes across the U.S.
REFERENCES
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services. 2017.
- Statistics about diabetes: Diagnosing diabetes and learning about prediabetes. American Diabetes Association. http://www.diabetes.org/diabetes-basics/statistics/
- Whitley HP, Yong EV, Rasinen C. Selecting an A1C Point-of-Care Instrument. Diabetes Spectrum. 2015; 28(3): 201-208.
- WHO guidelines on drawing blood: best practices in phlebotomy. World Health Organization. 2010.
- Fruhstorfer H, Schmelzeisen-Redeker G, Weiss T. Capillary blood sampling: relation between lancet diameter, lancing pain and blood volume. Eur J Pain. 1999; 3(3): 283-286.
- Grady M, Pineau M, Pynes MK, Katz B, Ginsberg B. A Clinical Evaluation of Routine Blood Sampling Practices in patients with Diabetes: Impact on Fingerstick Blood Volume and Pain. J Diabetes Sci Technol 2014. 8(4): 691-698.
About the Author