The inflammasome — a protein signaling network that is activated to rid the body of virus or bacteria-infected cells — may play an important role in triggering an immune response to cancer and causing an existing class of drugs to work better against cancers, according to a press release from Johns Hopkins Medicine.
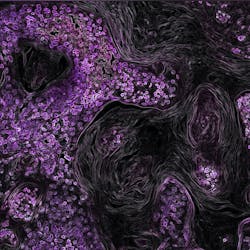
A collaborative research study led by experts at the Johns Hopkins Kimmel Cancer Center and University of Maryland Marlene and Stewart Greenebaum Cancer Center found that the inflammasome imparts a DNA repair defect-like state in cancer cells. In laboratory and animal models of ovarian and breast cancer cells, it induced an immune activating signal that directly made the cells susceptible to treatment with drugs called PARP inhibitors, drugs that disable the cancer cell’s ability to repair DNA damage caused by anticancer therapies. As a result, the cancer cell dies.
The findings, published online May 26 in the Proceedings of the National Academy of Sciences, appear to apply across multiple tumor types and create the potential for a wider use of PARP inhibitors.
In laboratory models, the researchers used the epigenetic drug 5-azacytidine to induce transcriptional BRCAness in two-thirds and one-third of ovarian and triple negative breast cancer cell lines tested. These BRCAness data were correlated with inflammasome activation in two cell lines, which demonstrated the most marked induction of BRCAness.
The drug 5-azacityidine is classified as a demethylating agent because it blocks a chemical process known as DNA methylation and can restore function to some cancer suppressor genes. Ongoing research also studies the ability of this drug, and other epigenetic drugs, to prime cancer cells for a better response to immunotherapies.
Turning the inflammasome on with epigenetic therapy, makes cancer cells targets of the immune system and responsive to drugs known as PARP inhibitors, the researchers said.
BRCA mutations alter the body’s ability to repair DNA, putting those affected at higher risk of developing breast, ovarian, pancreas and other cancers. However, cancers—particularly breast and ovarian cancers—that contain BRCA mutations often respond to treatment with PARP inhibitors, which disable the cancer cell’s ability to repair damage caused by anticancer drugs and radiation therapy.
“This mutation is present in only a small percentage of patients with breast and ovarian cancers, and this is the only setting where PARP inhibitors have demonstrable clinical efficacy,” says co-author Stephen Baylin, MD, Virginia and D.K. Ludwig Professor for Cancer Research.
Using 5-azacytidine to make cancer cells, which do not have BRCA mutations act like they have the mutations—a situation the researchers refer to as “BRCAness”—sensitizes cancer cells to treatment with PARP inhibitors and may expand the benefit of the drug to more patients.
The researchers also explain that a pathway called STING (stimulator of interferon genes) is a key regulator of the inflammasome. STING, shown to convert cold tumors, or tumors that do not attract the attention of the immune system, into hot tumors, ones that are most likely to respond to immunotherapies. STING causes CD8+ T cells to traffic to tumors and, in animal models, made breast cancer cells more responsive to immune checkpoint inhibitors.
In a surprising twist, the work of the investigators could potentially shed light on a severe and deadly inflammatory process, called cytokine storm syndrome (CSS), occurring in SARS-CoV-2 infection, the researchers say. They hypothesize that overactivation of the inflammasome may be a key regulator of CSS, the most severe complication of COVID-19 infection.