The evolution of Alzheimer’s disease diagnosis
Alzheimer’s disease (AD) is the most common cause of dementia in the elderly and is associated with a slow, progressive decline throughout the course of the disease, which eventually leads to a patient’s death generally within 5–12 years from symptom onset.1
AD and related dementias are characterized by neuropathological lesions in the brain. Amyloid plaques composed of extracellular deposition of β-amyloid (Aβ) and intraneuronal neurofibrillary tangles (NFTs) consisting of aggregated hyperphosphorylated and misfolded insoluble tau protein are both considered neuropathological hallmarks of AD. The presence of these neuropathological changes is necessary for a true AD diagnosis, and to-date the gold standard for AD diagnosis can only occur upon autopsy. Unfortunately, detecting early-stage Alzheimer’s disease in clinical practice can be challenging, mainly due to the vagueness of symptoms that can easily be dismissed as part of the normal aging process. However, diagnosing the disease (or risk of disease) early, allows both the individual and their caregivers to plan more effectively for the future, as well as to access treatments that can help manage symptoms.2
Cognitive testing
For the last 45 years, clinicians have relied primarily on cognitive assessment, including cognitive screening tests such as the Mini-Mental State Examination (MMSE) and more recently the Montreal Cognitive Assessment (MoCA), alongside a clinical workup to diagnose AD.3 The MMSE (or Folstein test) is a 30-point questionnaire extensively used in clinical and research settings to measure cognitive impairment, whereas the MoCA was developed as a tool to screen patients who present with mild cognitive complaints and usually perform in the normal range on the MMSE.4,5 While clinical diagnosis relying primarily on cognitive tests can reach 70% to 90% accuracy in late stages of AD, it is much less accurate in early stages of mild cognitive impairment (MCI) due to AD, and it is well known that MCI can have many pathological causes unrelated to AD.6,7 The inaccuracy of clinical diagnoses utilizing only cognitive tests to diagnose early AD has been observed by comparing neuropathological results after autopsy. In a longitudinal community-based clinical-pathologic study, 483 older persons underwent a battery of cognitive tests including the MMSE. Of the 179 persons diagnosed with probable AD, 88% were confirmed to have AD by pathologic criteria. However, when examining the 134 persons with MCI, the number of patients with pathologically confirmed AD was reduced to 54%, of which 59% had amnestic MCI and 49% non-amnestic MCI; despite the fact that amnestic MCI is often thought to be a more specific sign of early AD.7,8 This indicates that symptomology and cognitive tests alone cannot be used to reliably diagnose early AD.
In more recent years, the advent of neuroimaging including amyloid positron emission tomography (PET) and cerebrospinal fluid (CSF) testing have changed the dementia field, allowing a significant shift in the diagnostic framework from a clinical diagnosis (relying primarily on symptoms) to a purely biological definition of AD. This approach allowed AD to be viewed as a continuum that can be identified through the combination of biomarkers and neuropathological findings.
PET imaging
For the past 20 years, amyloid PET imaging has allowed visualization and quantification of insoluble Aβ protein fibrillary deposit, defining total load and spatial distribution of Aβ pathology.9 PET imaging of amyloid plaques can therefore identify patients destined to develop AD several years before the onset of dementia.10 PET imaging has accelerated the understanding of AD and related neurodegenerative disorders associated with cognitive impairment providing physicians with valuable information for patient’s diagnosis and management.11
The assessment of amyloid scans is based on the binding of fluorine-18 (F-18) amyloid tracers to cerebral cortical fibrillar amyloid, superficial to the nonspecific deep and subcortical white matter.11 Currently, three F-18 amyloid PET tracers (florbetapir, flutemetamol, and florbetaben) have been approved by the U.S. Food and Drug Administration (FDA) and European Medicines Agency for use in assessing amyloid pathology and have published sensitivities and specificities ranging from 82%–98% and 77%–95%, respectively.12–14
Two studies have looked at amyloid PET imaging and clinical diagnoses in patients with autopsy confirmation. In the first of these two studies that looked at 59 patients ranging from normal to dementia status, clinical evaluation had sensitivity of 72% (28/39) and specificity of 95% for neuropathologically confirmed AD. Amyloid PET corrected 10 of 11 clinical false negatives and one clinical false positive, but miscategorized 2 of 28 clinical true positives.15,16 In the second study that included 57 patients with a clinical diagnosis of AD, three with dementia with Lewy bodies (DLB), six with other dementias, and eight without dementia, clinical evaluation had sensitivity of 94% (44/47) and specificity of 52% (14/27), whereas amyloid PET had sensitivity of 98% and specificity of 89%.17
Although amyloid PET allows for an accurate detection of amyloid plaques and thus a positive PET result raises confidence in the diagnosis of AD, amyloid PET scans are expensive and testing centers are not always easily accessible for the patient. Additionally, since amyloid PET commonly relies on visual assessment and interpretation of scans, the subjectivity of readers can cause variability in the accuracy of the diagnosis.
CSF biomarkers
In the last decade, the availability of cerebrospinal fluid (CSF) biomarkers has offered an informative and relatively non-invasive look into ongoing pathological changes in the brain, allowing in vivo detection of neurodegeneration associated with AD, and thus representing an important tool in both research and in the clinical practice for early AD diagnosis.18 CSF serves as mechanical and immunological protection for the brain, and since CSF is in direct contact with the extracellular spaces of the brain, CSF can better reflect its biochemical changes (including the metabolism of Aβ and tau proteins).19
When evaluating the AD continuum, reduced soluble Aβ1–42 levels in the CSF and increased uptake of F-18 amyloid tracers are used as in vivo measurements of brain amyloid β accumulation.20 Lower level of Aβ1–42 in the CSF of patients with AD is a result of the peptide aggregation and deposition in the brain, as defined by the inverse correlation with plaque load in cortical regions.21–23 Furthermore, CSF Aβ1–42 concentrations have shown high concordance with plaque burden at autopsy as well as PET brain scans.24 Interestingly, in cohorts with higher proportion of asymptomatic subjects, circa 10%–20% of the subjects may show discordant results (i.e., CSF+/PET-), indicating that the abnormal accumulation of Aβ in pre-clinical AD patients can be detected earlier with CSF Aβ1-42 compared to amyloid PET.25–28
CSF amyloid Aβ1-42/Aβ1-40 ratio
When considering CSF amyloid levels for the assessment of amyloidosis in the context of early AD onset, important considerations need to be made. Amyloid production is known to vary from individual to individual. Therefore, healthy individuals with relatively low total Aβ might be misdiagnosed as having ‘pathologically low’ Aβ1-42 concentrations leading to misdiagnoses in circa 5%–10% of cases when Aβ1-42 is used as the sole amyloid biomarker.29 CSF Aβ1-40 can be used to normalize CSF Aβ1-42 levels with the introduction of the Aβ1-42/Aβ1-40 ratio. This approach improves AD diagnosis by minimizing interindividual differences in CSF Aβ levels. Furthermore, Aβ1-40 is less prone to aggregation and can normalize amyloid loss due to the tendency of amyloid to adsorb to surfaces during CSF collection and measurement, thereby reducing preanalytical and analytical variabilities between laboratories.30,31 Due to the normalization of both interindividual amyloid production and preanalytical variability, the Aβ1-42/Aβ1-40 ratio consistently improves concordance with amyloid PET compared to levels of Aβ1-42 alone.32
On May 4, 2022, the FDA granted marketing authorization of the first in vitro diagnostic test for the assessment of β-Amyloid pathology in patients being evaluated for AD and other causes of cognitive decline.33 This test, which measures CSF Aβ1-42/Aβ1-40, is intended to be used in adults 55 years of age and older presenting with cognitive impairment who are being evaluated for AD and other causes of cognitive decline.
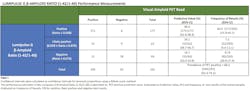
In the clinical evaluation study of 292 CSF samples from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) sample bank, 96.6% of individuals with positive results from this test had the presence of amyloid plaques by amyloid PET scan, and 83.9% of individuals with negative results had a negative amyloid PET scan (Table 1).
This test offers an alternative for patients to determine their brain amyloid status while providing clinicians with the same information as a PET scan. CSF testing could typically be completed the same day significantly reducing time and costs associated with PET imaging, as well as eliminating patient’s exposure to radiation.
Conclusion
The use of cognitive assessment tools that rely primarily on patient’s symptoms as a stand-alone test significantly limits the possibility of a reliable diagnosis of early AD. In recent years, the advances in neuroimaging and the development of accurate CSF AD biomarker tests have helped to better understand the early pathological changes occurring in the AD brain. Such advances can serve as a robust tool for the detection of early stages of AD, years before the onset of dementia. The potential of an early diagnosis facilitates clinical trial enrollment for new AD therapies and enables patients and their doctors to make more informed decisions and take action much earlier in the disease process.
References
- Long JM, Holtzman DM. Alzheimer Disease: An Update on Pathobiology and Treatment Strategies. Cell. 2019;179(2):312-339. doi:10.1016/j.cell.2019.09.001.
- Porsteinsson AP, Isaacson RS, Knox S, Sabbagh MN, Rubino I. Diagnosis of Early Alzheimer’s Disease: Clinical Practice in 2021. J Prev Alzheimer’s Dis. 2021;8(3):371-386. doi:10.14283/jpad.2021.23.
- Dubois B, Villain N, Frisoni GB, et al. Clinical diagnosis of Alzheimer’s disease: recommendations of the International Working Group. Lancet Neurol. 2021;20(6):484-496. doi:10.1016/S1474-4422(21)00066-1.
- Creavin, S. T., Wisniewski, S., Noel-Storr, A. H., Trevelyan, C. M., Hampton, T., Rayment, D., Thom, V. M., Nash, K. J. E., Elhamoui, H., Milligan, R., Patel, A. S., Tsivos, D. v., Wing, T., Phillips, E., Kellman, S. M., Shackleton, H. L., Singleton, G. F S. Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev. 2016;(1). doi:10.1002/14651858.CD011145.pub2.
- Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695-699. doi:10.1111/j.1532-5415.2005.53221.
- Breton A, Casey D, Arnaoutoglou NA. Cognitive tests for the detection of mild cognitive impairment (MCI), the prodromal stage of dementia: Meta-analysis of diagnostic accuracy studies. Int J Geriatr Psychiatry. 2019;34(2):233-242. doi:10.1002/gps.5016.
- Schneider, Julie A. Arvanitakis, Z. Leurgans, S.E. Bennet DA. The Neuropathology of Probable Alzheimer’s Disease and Mild Cognitive Impairment. Ann Neurol. 2009;66(2):200-208. doi:10.1002/ana.21706.
- Salmon DP. Neuropsychological features of mild cognitive impairment and preclinical alzheimer’s disease. Curr Top Behav Neurosci. 2011;(10):187-212. doi:10.1007/7854.
- Palmqvist S, Zetterberg H, Mattsson N, et al. Detailed comparison of amyloid PET and CSF biomarkers for identifying early Alzheimer disease. Neurology. 2015;85(14):1240-1249. doi:10.1212/WNL.0000000000001991.
- Varghese T, Sheelakumari R, James JS MP. A review of neuroimaging biomarkers of Alzheimer’s disease. Neurol Asia. 2013;18(3):239-248. Accessed July 22, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4243931/.
- Weidman D. Limitations of Amyloid Imaging in Alzheimer’s Disease. Elsevier Inc.; 2020. doi:10.1016/b978-0-12-815868-5.00031-1.
- AS GH. VIZAMYL flutemetamol (18F) Package Leaflet. Published online 2019. doi:10.1016/b978-0-08-023447-2.50022-x.
- Eli Lilly Nederland. Amyvid florbetapir (18F) Package Leaflet. Published online 2017. doi:10.2307/j.ctv1q26vdb.13.
- GmbH LRB. Neuraceq -florbetaben (18F) Package leaflet. Published online 2018. doi:10.1016/b978-0-08-023447-2.50022-x.
- Clark CM, Pontecorvo MJ, Beach TG, et al. Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-β plaques: A prospective cohort study. Lancet Neurol. 2012;11(8):669-678. doi:10.1016/S1474-4422(12)70142-4.
- Fink HA, Hemmy LS, Linskens EJ, et al. Key Question 2: Biomarkers for Identifying Neuropathologically Confirmed AD. Agency for Healthcare Research and Quality; 2020. Published online 2020. Accessed July 22, 2022. https://www.ncbi.nlm.nih.gov/books/NBK556551/.
- Sabri O, Sabbagh MN, Seibyl J, et al. Florbetaben PET imaging to detect amyloid beta plaques in Alzheimer’s disease: Phase 3 study. Alzheimer’s Dement. 2015;11(8):964-974. doi:10.1016/j.jalz.2015.02.004.
- Spallazzi M, Barocco F, Michelini G, et al. CSF biomarkers and amyloid PET: concordance and diagnostic accuracy in a MCI cohort. Acta Neurol Belg. 2019;119(3):445-452. doi:10.1007/s13760-019-01112-8.
- Hameed S, Fuh J-L, Senanarong V, et al. Role of Fluid Biomarkers and PET Imaging in Early Diagnosis and its Clinical Implication in the Management of Alzheimer’s Disease. J Alzheimer’s Dis Reports. 2020;4(1):21-37. doi:10.3233/adr-190143.
- Mattsson N, Insel PS, Donohue M, et al. Independent information from cerebrospinal fluid amyloid-β and florbetapir imaging in Alzheimer’s disease. Brain. 2015;138(3):772-783. doi:10.1093/brain/awu367.
- Ikonomovic MD, Klunk WE, Abrahamson EE, et al. Post-mortem correlates of in vivo PiB-PET amyloid imaging in a typical case of Alzheimer’s disease. Brain. 2008;131(6):1630-1645. doi:10.1093/brain/awn016.
- Mollenhauer B, Esselmann H, Roeber S, et al. Different CSF β-amyloid processing in Alzheimer’s and Creutzfeldt-Jakob disease. J Neural Transm. 2011;118(5):691-697. doi:10.1007/s00702-010-0543-z.
- Tapiola T, Alafuzoff I, Herukka SK, et al. Cerebrospinal fluid β-amyloid 42 and tau proteins as biomarkers of Alzheimer-type pathologic changes in the brain. Arch Neurol. 2009;66(3):382-389. doi:10.1001/archneurol.2008.596.
- Korecka M, Figurski MJ, Landau SM, et al. Analytical and Clinical Performance of Amyloid-Beta Peptides Measurements in CSF of ADNIGO/2 Participants by an LC-MS/MS Reference Method. Clin Chem. 2020;66(4):587-597. doi:10.1093/clinchem/hvaa012.
- Cairns NJ, Ikonomovic MD, Benzinger T, et al. Absence of Pittsburgh compound B detection of cerebral amyloid β in a patient with clinical, cognitive, and cerebrospinal fluid markers of Alzheimer disease: A case report. Arch Neurol. 2009;66(12):1557-1562. doi:10.1001/archneurol.2009.279.
- Fagan AM, Mintun MA, Shah AR, et al. Cerebrospinal fluid tau and ptau181 increase with cortical amyloid deposition in cognitively normal individuals: Implications for future clinical trials of Alzheimer’s disease. EMBO Mol Med. 2009;1(8-9):371-380. doi:10.1002/emmm.200900048.
- Mattsson N, Insel PS, Landau S, et al. Diagnostic accuracy of CSF Ab42 and florbetapir PET for Alzheimer’s disease. Ann Clin Transl Neurol. 2014;1(8):534-543. doi:10.1002/acn3.81.
- Palmqvist S, Mattsson N, Hansson O. Cerebrospinal fluid analysis detects cerebral amyloid-β accumulation earlier than positron emission tomography. Brain. 2016;139(4):1226-1236. doi:10.1093/brain/aww015.
- Hansson O, Lehmann S, Otto M, Zetterberg H, Lewczuk P. Advantages and disadvantages of the use of the CSF Amyloid β (Aβ) 42/40 ratio in the diagnosis of Alzheimer’s Disease. Alzheimer’s Res Ther. 2019;11(1):1-15. doi:10.1186/s13195-019-0485-0.
- Delaby C, Muñoz L, Torres S, et al. Impact of CSF storage volume on the analysis of Alzheimer’s disease biomarkers on an automated platform. Clin Chim Acta. 2019;490(December 2018):98-101. doi:10.1016/j.cca.2018.12.021.
- Vanderstichele HMJ, Janelidze S, Demeyer L, et al. Optimized Standard Operating Procedures for the Analysis of Cerebrospinal Fluid Aβ42 and the Ratios of Aβ Isoforms Using Low Protein Binding Tubes. J Alzheimer’s Dis. 2016;53(3):1121-1132. doi:10.3233/JAD-160286.
- Alcolea D, Pegueroles J, Muñoz L, et al. Agreement of amyloid PET and CSF biomarkers for Alzheimer’s disease on Lumipulse. Ann Clin Transl Neurol. 2019;6(9):1815-1824. doi:10.1002/acn3.50873.
- FDA permits marketing for new test to improve diagnosis of Alzheimer’s disease. U.S. Food and Drug Administration. Accessed July 22, 2022. https://www.fda.gov/news-events/press-announcements/fda-permits-marketing-new-test-improve-diagnosis-alzheimers-disease
About the Author

Rianne Esquivel, PhD
Serves as US Scientific Affairs Manager at Fujirebio Diagnostics Inc. Leading the department’s neurodegenerative disease program, Rianne initiates and manages protocols to develop clinical evidence for Fujirebio’s current biomarker portfolio. She also investigates new technologies and novel biomarkers.

Francesca I. De Simone, PhD
is a scientific affairs specialist at Fujirebio Diagnostics.