Shining renewed light on a tried-and-true test: The critical role of osmolality in improving health outcomes in patients with hyponatremia
Hyponatremia is often observed at admission but also frequently develops during hospitalization either as a complication of an underlying illness or as the result of therapeutic interventions.8 High incidences of hyponatremia have been reported in a variety of patient populations including those with heart failure,9,10 renal disease,11,12 cirrhosis,13 cancer,14,15,16 pneumonia,17 and stroke.18,19 Hyponatremia also frequently occurs after various surgical procedures including pelvic,20 spinal,21 and pituitary surgery.22,23 It is particularly prevalent in the elderly, in part because of age-related decline in renal function.24,25 Additionally, patients who receive maintenance intravenous fluids, particularly children, are in danger of developing hyponatremia.26,27 Hyponatremia is also common with COVID-19, occurring in nearly a third of hospitalized patients.28,29
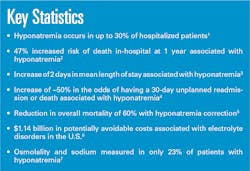
Association of hyponatremia with poor outcomes
Numerous studies have demonstrated the association between hyponatremia and poor outcomes across diverse patient populations.30,31,32,33 Winzeler et al. conducted a prospective observational 12-month follow-up study of 281 patients with profound hyponatremia (<125 mmol/L). During the follow-up period, 20.6% of patients died, 56.2% were rehospitalized at least once, and 42.7% had recurrent hyponatremia. However, it is not just severe hyponatremia that has been associated with adverse outcomes. Both mild (130–135 mmol/L) and moderate (125–129 mmol/L) hyponatremia have also been associated with unfavorable outcomes in the literature.2,34 In a meta-analysis of 81 published studies encompassing 850,222 patients, Corona et al. demonstrated that moderate hyponatremia is associated with an increased risk of mortality, and that it is a negative prognostic factor across multiple commonly observed clinical conditions, such as myocardial infarction, heart failure, cirrhosis, and pulmonary infections. Waikar et al. investigated in-hospital, 1-year and 5-year mortality in a prospective cohort study of 98,411 hospitalized adults and found that patients with hyponatremia had an increased risk of death in-hospital at 1 year (47%) and 5 years (25%). The increased risk of death was evident even in those with mild hyponatremia (37%) and was pronounced in patients admitted with cardiovascular disease, metastatic cancer, and those admitted for procedures related to the musculoskeletal system.2Poor outcomes have also been reported in COVID patients with hyponatremia of varying severity levels.28,35 In a retrospective, multicenter, observational cohort study, Frontera et al. identified the impact of mild, moderate, and severe admission hyponatremia on outcomes among COVID patients and reported that each level of worsening hyponatremia conferred 43% increased odds of in-hospital death. Further, the authors observed that hyponatremia was an independent predictor of in-hospital mortality and was associated with increased risk of encephalopathy and mechanical ventilation. Similarly, Carvalho et al. conducted a retrospective study of 296 adult patients with a diagnosis of COVID-19 and reported that ICU admission, mechanical ventilation, and death were significantly more frequent in hyponatremic patients compared to normonatremic patients (37% versus 14%; 17% versus 6%; 18% versus 9%).
Osmolality is well-established in the clinical pathway for hyponatremia
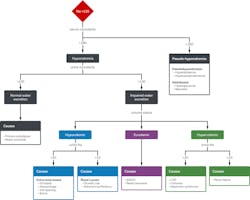
Correction of hyponatremia first requires proper diagnosis. The common electrolyte disorder is classified as hypoosmolar, isoosmolar, or hyperosmolar. Understanding the underlying cause of hyponatremia is important as the treatment options vary widely from fluid resuscitation for hyponatremia driven by volume depletion to volume restriction for hyponatremia driven by the syndrome of inappropriate antidiuretic hormone secretion (SIADH).37,38 It is important to cast a wide net in the initial workup of hyponatremia because patients may present with minimal information regarding relevant medical conditions or recent triggering events.39 Interpreting various laboratory parameters, including serum and urine osmolality, is necessary to differentiate between the various causes of hyponatremia and ensure proper patient management.40
Criteria for diagnosing hyponatremia is well-established.1,7,41,42 Measurement of serum osmolality is the first step in the laboratory diagnosis of hyponatremia, and if the test suggests a hypo-osmolar state, then urine osmolality helps determine whether the ability of the kidneys to dilute urine is intact (Figure 2).39
The utility of osmolality has also been recognized in the management of COVID patients due to the prevalence of hyponatremia in this patient population.43,44,45 O’Shea et al. published a COVID test menu for clinical laboratories that includes osmolality testing due to the potential for acute kidney injury in these patients. Similarly, Martinez et al. published guidance recommending daily monitoring of osmolality for inpatients during the acute phase of COVID-19.
Osmolality testing for proper patient management
Osmolality is a proven and medically necessary test in the management of hypontremia. Failure to measure plasma and urine osmolality in cases of hypontremia has been associated with increased mortality.45,46 In a retrospective study of adult patients with severe hyponatremia, Whyte et al. reported that 30% of patients died when neither serum nor urine osmolality was measured compared to 9.8% when both tests were measured.45 Similarly, Vaduganathan et al. analyzed serum osmolality measured at discharge in 3,744 patients hospitalized for heart failure and concluded that low discharge serum osmolality was independently predictive of worse discharge mortality and readmission.46
Knowledge and interpretation of a patient’s osmolality in cases of hyponatremia enable the physician to differentiate between the various causes of the electrolyte disorder and appropriately direct treatment. This is a critical issue because treatment varies drastically based on symptoms and underlying causes. Hyponatremia is treated with fluid restriction (in the setting of euvolemia), isotonic saline (in hypovolemia), and diuresis (in hypervolemia).47 Lack of osmolality testing makes diagnostic accuracy and subsequent treatment uncertain putting hyponatremic patients at risk.
Underutilization of osmolality impedes management of hyponatremia
Despite published guidance on its diagnosis, clear associations with poor outcomes and increased medical costs, and significant evidence that correcting hyponatremia is associated with improved outcomes and lower costs, hyponatremia is insufficiently investigated or overlooked entirely, and critical testing is not routine impacting patient treatment.36,48,49,50
Inadequate requisition of serum and urine osmolality is frequent in cases of hyponatremia. In a multicenter, retrospective, observational study, Tzoulis et al. found that only 23% of patients with hyponatremia had measurements of paired serum and urine osmolality and sodium.50 The study from Tzoulis et al. is not an outlier; numerous publications in the literature have consistently reported underutilization of measured osmolality in the investigation of hyponatremia.29,35,51,52,53
Huda et al. evaluated the assessment and management of hyponatremia in a large teaching hospital and found that adequate investigations were rarely performed. In fact, plasma osmolality was measured in only 26% of patients with severe hyponatremia and urine osmolality was measured in only 27%. The authors observed that treatment was often illogical with significant management errors in 33% of cases. Errors included, but were not limited to, inadequate investigation which could have changed management, treatment with fluid restriction plus intravenous saline, and diuretic induced hyponatremia treated with fluid restriction. Further, mortality was significantly higher in the group with management errors (41% versus 20%). The authors suggest that more appropriate management may have reduced the overall mortality rate. Additionally, they found a trend towards more efficient normalization of serum sodium concentrations in the appropriately managed group, deemed appropriate based on standards for the major diagnostic criteria of hyponatremia.51 Seo et al. reported similar management errors as Huda et al. The authors highlighted the importance of osmolality test results in guiding therapy.47
Even SIADH, the most common cause of hyponatremia, is often diagnosed without attention to the accepted diagnostic criteria.7,29,52,53 Greenberg et al. conducted an analysis of adult patients in the Hyponatremia Registry from 225 sites in the United States and European Union and observed that only 47% of 1,524 patients with an assigned diagnosis of SIADH had all three cardinal tests (serum osmolality, urine osmolality, and serum sodium) performed and 11% had none. Serum osmolality was measured in 66% of patients and urine osmolality in 68%.52 Burst et al. studied smaller subsets of the Hyponatremia Registry. The authors analyzed 358 cancer patients with a clinical diagnosis of SIADH and similarly found that only 46% of patients had all three tests performed, and 13% had none. They reported that test underutilization was even more pronounced in subgroups including lung cancer patients and small cell lung cancer patients with all tests performed in only 41% and 36% of patients respectively.53
Diagnostic rigor appears to be even worse in COVID patients. In a retrospective, multicenter, observational cohort study of hospitalized patients with laboratory-confirmed SARS-CoV-2, Frontera et al. attempted to determine the etiology of hyponatremia but were unsuccessful because serum and urine osmolality were available in less than 15% of the cohort.29 Yen et al. reported that serum and urine osmolality measurements were available as part of admission hyponatremia workup tests in only 18% and 12% of cases respectively. Further, the authors reported that serum and urine osmolality were only ordered on the day of admission, when hyponatremia was identified, in 9% and 5.4% of cases respectively.54 Similarly, Carvalho et al. reported that osmolality was rarely measured in a noninterventional retrospective cohort of patients with mild hyponatremia and COVID-19.35
Osmolality is a cost-effective test with a significant return on investment
Not performing osmolality testing is potentially harmful to the patient, but it is also very expensive given that some of the medications now available to treat SIADH cost $500–$1,000 per day. Just one or two misdiagnosed patients can cost the hospital system as much as the price of an osmometer, the device used to measure osmolality. This does not include the possible costs arising from litigation for malpractice due to misdiagnosis and improper treatment.55 Further, cost per test is highly inexpensive and reimbursement for the test is well-established.46,56,57
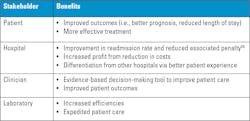
The College of American Pathologists (CAP) estimated the value generation potential of proper laboratory testing of electrolyte disorders based on Prometheus data and fluid and electrolyte disorders represented 1.5 percent of all potentially avoidable costs. When scaled to the national level and expanded beyond the commercial population based on the CAP’s modeling, this represents potential avoidable costs of $1.14 billion nationally.6 Implementing osmolality testing as standard of care in patients with hyponatremia could help optimize proper patient management to avoid unfavorable outcomes and enable hospitals to recover a significant portion of the $1.14 billion in potentially avoidable costs associated with electrolyte disorders in the United States. Figure 3 outlines the benefits of osmolality testing to stakeholders in the circle of care.Conclusion
In summary, hyponatremia represents a significant medical burden that is prevalent in various patient populations. Despite published guidance on its diagnosis, clear associations with poor outcomes, increased medical costs, and significant evidence that correcting hyponatremia is associated with improved outcomes, the common electrolyte disorder is often inadequately investigated or ignored. Osmolality testing is proven and medically necessary to effectively manage hyponatremia, improving outcomes and reducing excess resource utilization. However, osmolality is underutilized even though the cost per test is low, the test is classified as ‘urgent,’ and osmometers are well-established medical devices.58
When clinicians have a clear understanding of the importance of determining the etiology of hyponatremia, and the utility of measuring osmolality to do so, it follows that they would be more likely to order the test. Osmolality testing combined with education on interpreting test results are both critical in addressing suboptimal management of hyponatremia. The return on investment would be substantial due to the low cost per test and $1.14 billion in potentially avoidable costs associated with electrolyte disorders in the United States alone. Addressing underutilization of osmolality testing in cases of hyponatremia, including education of ordering providers, is the first step in ensuring that everyone who needs an osmolality test gets one.
References
About the Author

Julie MacKenzie, MBA
is Senior Manager, Clinical Product Portfolio at Advanced Instruments, LLC. She has been with Advanced Instruments for over 14 years. She received her Bachelor’s degree in Biochemistry, Cellular, and Molecular Biology from Connecticut College and she earned her MBA from Boston College. She is passionate about improving quality of care.