Urinary casts: Indicators of underlying clinical pathology
To take the January CE test online go HERE. For more information, visit the Continuing Education tab.
LEARNING OBJECTIVES
Upon completion of this article, the reader will be able to:
1. List disease statistics of CKD in the global and U.S. populations.
2. Discuss the function and parts of the renal system.
3. Identify and define the components of a urinalysis.
4. Discuss key findings in a urinalysis that help to diagnose CKD.
The kidneys, two fist-sized, bean-shaped organs, reside just below the rib cage in the back of the abdomen under the liver. Properly functioning kidneys are essential for maintaining overall health. Unfortunately, for millions of people around the world, kidney diseases interrupt kidney function, leading to high morbidity and mortality.
Kidney disease
Chronic kidney disease (CKD), the most common type of kidney disease, occurs slowly over a long period of time, getting progressively worse. Currently, an estimated 13.4% of the global population is affected by CKD at all stages and 10.6% for moderate to advanced stages.1 Globally, kidney diseases have risen from the world’s 13th leading cause of death to the 10th, and mortality has increased from 813,000 in 2000 to 1.3 million in 2019.2 Over 6 million adults have been diagnosed with CKD in the United States alone, where it is also the 10th leading cause of death.3
Structural changes, genetics, and comorbidities all may play a role in determining CKD risk. More than 30% of adults with diabetes and 20% of adults with hypertension may have CKD.4 Other causes include heart disease, obesity, and a family history of kidney failure.5
One of the challenges with identifying and treating CKD, is that early disease is often without symptoms—90% of patients don’t know that their kidneys are damaged.6 Fortunately, most cases of CKD can be detected by simple urine and blood tests. As with most medical conditions, early detection leads to better patient outcomes.6
The renal system
The kidneys, along with the ureters, bladder, and urethra, comprise the renal system. Kidneys serve several vital functions—they filter blood to remove wastes and toxins, remove excess water from the bloodstream and produce renin to help maintain blood pressure, produce erythropoietin to maintain a healthy level of red blood cells, balance salts in the body, and convert dietary vitamin D to its biologically active form, calcitriol, to regulate calcium. Kidneys filter about 200 quarts of fluid every day; 99% of that fluid is reused in the body, while the remaining 1% is converted to urine.7
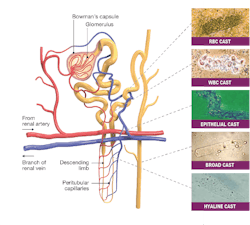
Unfiltered blood enters the kidney through the renal artery, which then branches into progressively smaller blood vessels until it reaches one of the more than 1 million nephrons in the kidney. Nephrons are the microscopic functional unit of the kidney, and each is comprised of a nephron and a tubule. (See Figure 1.) Inside the nephron, the glomerulus, a network of capillaries enclosed within a sac (Bowman’s capsule), filters water and solutes from the blood. Smaller molecules, wastes, and fluids pass through the glomerulus and into the tubules, which ultimately feed into the Loop of Henle, a U-shaped structure where water and sodium chloride are resorbed from the filtrate. Larger molecules and cells stay in the blood.8 Wastes from the filtrate exit as concentrated urine through the ureter to the bladder and filtered blood returns to the body via the renal vein.
CKD and other kidney diseases can be identified on urinalysis. Acute kidney disease (AKI), which occurs over days or even hours, results in the retention of nitrogenous wastes. Kidney stones and pyelonephritis (kidney infection) both cause severe pain. Nephrotic syndrome presents with heavy proteinuria and lipuria. Others include glomerulonephritis, autoimmune conditions, kidney stones, and polycystic kidney disease.
Urinalysis
Laboratory testing can provide timely information for identification and comprehensive therapeutic interventions to help drastically improve patient outcomes. Cost-effective9 and usually noninvasive,10 urinalysis provides critical information in the early detection of many diseases, including kidney disease. Considered to be the first developed laboratory test,10 routine urinalysis can be used to screen for underlying health conditions such as diabetes, urinary tract infections, and kidney disease. It can also be used to monitor disease and disease treatment.
The three main components of urinalysis are macroscopic examination of the sample, chemical analysis, and microscopic examination of the urine sediment. Additional tests including microbiology and cytology may also be performed. The presence of crystals, casts, and blood cells in the urine sediment provides vital information for both diagnosis and prognosis.
Macroscopic examination
Macroscopic evaluation of urine is simply a visual examination. Macroscopic analysis of urine is done by visually inspecting the physical appearance of the urine. Normal urine is light yellow and clear. Macroscopic urinalysis notes the amount, color, and clarity of the urine as well as any other visible characteristics of the urine such as the presence of blood or blood clots, precipitates, or sediments.
Unusual colors may indicate infection, liver dysfunction, or drug use,11 while turbidity may suggest infection or the presence of RBCs.12
Urine chemistry
Done to measure levels of certain substances such as proteins, sugars, ketone, and bilirubin, urine chemistry can be used to help diagnose and monitor a variety of health conditions including diabetes, urinary tract infections, and kidney disease.
CKD is divided into five stages based on the estimated glomerular filtration rate (eGFR) and urine albumin-creatinine ratio (uACR). Albumin, a protein normally found in the blood, is involved in building muscles, repairing tissues, and fighting infections. In a normal kidney, albumin cannot pass through the kidney’s filter and into the urine, but in a diseased kidney, albumin leaks through the filter. Creatinine is a waste product of protein metabolism—from food or from normal muscle cell turnover and is normally found in both serum and urine. If the kidneys are not functioning properly, the urine level of creatinine decreases. To ensure that the urine concentration doesn’t interfere with the determination of albumin levels, the uACR test is done. The uACR is a ratio between urine albumin and serum creatinine; a uACR greater than 30 mg(albumin)/g(creatinine) is indicative of albuminuria—excessive protein in the urine.13 eGFR is a calculation based on serum creatinine levels and shows how well the kidneys are filtering toxins and wastes from the blood.14 A normal eGFR is above 60 mL/min/1.73m2, and a normal uACR is below 30 mg/g.14 Falling eGFR numbers and rising uACR numbers are indicators of progressing disease.
Urine microscopy
Urine microscopy is a common test in the clinical laboratory and is used to evaluate cells, casts, and crystals in the urine. While it is not uncommon to find some epithelial cells in the urine, an increased number may be a sign of trauma, inflammation, or infection in the urinary tract. Similarly, bacterial or yeast in the sample suggest an underlying renal system infection. Blood cells in the urine may be benign—for example, as a result of heavy exercise—but may also indicate a more serious disorder such as a severe infection or urinary tract cancer.15 The presence of urine casts often portend a more serious underlying kidney condition and may be one of the first early indicators of underlying kidney disease.
Casts
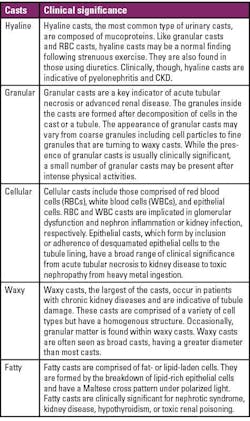
Urinary casts are cylindrical mucoprotein particles that arise from the distal convoluted tubule or collecting duct during periods of urinary concentration or stasis. All casts have a core matrix glycoprotein, uromodulin, that is secreted by renal tubular cells in the ascending arm of the Loop of Henle.12 Trapped contents in the tubule lumen intermix with the uromodulin, and eventually, the tubule-shaped cast is excreted in the urine. Different casts are comprised of different components and are formed in different areas of the tubule (See Figure 1), which may be helpful in determining clinical significance. Urine cast formation is influenced by the pH, concentration, and temperature of the urine—as well as by the presence of drugs or underlying genetic conditions.
And while having some casts in the urine sediment may be normal, the type and number of casts may indicate the presence of renal disease12 and can be detected and characterized using automated urinalysis. The clinical significance of some of the most common casts is shown in Table 1 below.
Conclusion
Advancements in automation are streamlining the urinalysis laboratory workflow and improving laboratory efficiency to take the subjectivity out of urinalysis. Integrated automated urinalysis systems with automated urine microscopy and auto-particle recognition software provide numeric counts and digital image results and can also auto-classify particles based on size, shape, contrast, and texture and assist with particle sub-categorization. The insights gained from urinalysis with sensitive cast identification are facilitating partnerships between laboratorians and clinicians to identify kidney disease in a timely manner—allowing them to focus their time on the most critical patients.
References
1. Hill NR, Fatoba ST, Oke JL, et al. Global Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-Analysis. PLoS ONE. 2016;11(7):e0158765. doi:10.1371/journal.pone.0158765.
2. World Health Organization. The Top 10 Causes of Death. Fact Sheet | The Top 10 Causes of Death. December 9, 2020. Accessed October 31, 2023. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
3. National Center for Health Statistics. FastStats - Kidney Disease. Center for Disease Control and Prevention. January 17, 2023. Accessed November 1, 2023. https://www.cdc.gov/nchs/fastats/kidney-disease.htm.
4. Diabetes and Chronic Kidney Disease . Centers for Disease Control and Prevention. December 30, 2022. Accessed November 7, 2023. https://www.cdc.gov/diabetes/managing/diabetes-kidney-disease.html.
5. National Institute of Diabetes and Digestive and Kidney Diseases. Chronic Kidney Disease (CKD) - NIDDK. Accessed November 7, 2023. https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd.
6. National Kidney Foundation. Kidney Disease: The Basics. Kidney Disease: The Basics. 2023. Accessed November 2, 2023. https://www.kidney.org/news/newsroom/fsindex.
7. National Kidney Foundation. Top 5 Jobs Kidneys Do. 2023. Accessed November 3, 2023. https://www.kidney.org/kidneydisease/top-5-jobs-kidneys-do.
8. NIH. Your Kidneys & How They Work - NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. June 2018. Accessed October 31, 2023. https://www.niddk.nih.gov/health-information/kidney-disease/kidneys-how-they-work.
9. Cusick MM, Tisdale RL, Chertow GM, Owens DK, Goldhaber-Fiebert JD. Population-Wide Screening for Chronic Kidney Disease : A Cost-Effectiveness Analysis. Ann Intern Med. 2023;176(6):788-797. doi:10.7326/M22-3228.
10. Queremel Milani DA, Jialal I. Urinalysis. In: StatPearls. StatPearls Publishing; 2023.
11. Roxe DM. Urinalysis. In: Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Butterworths; 1990.
12. Brunzel NA. Fundamentals of Urine & Body Fluid Analysis. 4th ed. (Bellinger KG, Briski M, Crawford C, et al., eds.). Elsevier; 2018.
13. National Institute of Diabetes and Digestive and Kidney Diseases. Urine Albumin-to-Creatinine Ratio (UACR) In Evaluating Patients with Diabetes for Kidney Disease. 2010. Accessed November 7, 2023. https://www.niddk.nih.gov/-/media/Files/Health-Information/Health-Professionals/Kidney-Disease/UACRQuickReferenceSheet.pdf.
14. American Kidney Fund. Blood test: eGFR (estimated glomerular filtration rate) | American Kidney Fund. American Kidney Fund. October 27, 2023. Accessed October 31, 2023. https://www.kidneyfund.org/all-about-kidneys/tests/blood-test-egfr.
15. Johns Hopkins Medicine. Hematuria (Blood in the Urine). Johns Hopkins Medicine Conditions and Diseases. 2023. Accessed November 2, 2023. https://www.hopkinsmedicine.org/health/conditions-and-diseases/hematuria-blood-in-the-urine.
About the Author

Paul R. Morris, MD, MA
earned his medical degree from Boston University. He completed his residency in Pathology at Duke and fellowship in Blood Banking/Transfusion Medicine at the University of North Carolina. Dr. Morris has over twenty years of experience in blood and tissue banking, reference laboratories, and the in-vitro diagnostics industry. He currently is the Medical Director for Beckman Coulter Diagnostics and Life Sciences focusing on risk management and new product development.