Navigating the world of lab safety through standardized practices
Clinical laboratories are complex environments that depend on strong safety practices for their success. These practices include, but are not limited to, infection prevention and control, personal protective equipment, collection of patient samples, disposal of biological and other hazardous wastes, and staff education and training. Numerous federal agencies regulate the clinical lab: the Centers for Medicare & Medicaid Services (CMS), U.S. Food & Drug Administration (FDA), and Occupational Safety and Health Administration (OSHA). There are also numerous laboratory accreditation organizations; for example, AABB, American Association for Laboratory Accreditation, College of American Pathologists (CAP), COLA, and The Joint Commission. A leading source for clinical laboratory professionals is the Clinical and Laboratory Standards Institute (CLSI), which develops consensus standards and guidelines through committees comprised of clinical laboratory experts. Many of CLSI’s standards and guidelines provide the “how” for federal and accreditation requirements.
Medical Laboratory Observer (MLO) revisited our April 2022 Lab of the Year runner-up, Cincinnati Children’s Hospital Medical Center’s clinical laboratories. KathyIf a safety event does occur in the lab, Good stated, “Our labs have safety stations that include PPE cabinets, spill kits, and bloodborne pathogen response kits that are readily available with just-in-time information on how to use the infrequently used tools. The goal is to make it easy to do the right thing.”
In April 2022, CCHMC told us there are a number of sources that can and should be used to develop safety protocols. CCHMC’s clinical laboratories are CAP-accredited at nine physical locations. (CAP’s accreditation program uses the CLSI standards to develop its checklist requirements.) Because CCHMC is accredited by The Joint Commission, several laboratory locations are also subject to Joint Commission requirements for waived point-of-care testing. CCHMC’s labs also hold CLIA certificates, so they are subject to validation surveys by state surveyors for the CLIA regulations. And lastly, CCHMC has to follow FDA regulations for its blood transfusion services.1
CLSI guidelines for staff safety
CLSI standards are available to all laboratorians as guidance under many and varied circumstances, including basic laboratory safety, with specific instructions as to what to do when cases arise. Christopher told us that a fundamental aspect is personal protective equipment (PPE). “Various CLSI standards include the proper use of personal protective equipment, safety, and training.”
The most notable in this area is CLSI document M29-A4—Protection of Laboratory Workers from Occupationally Acquired Infections; Approved Guideline—Fourth Edition.2 This guideline is intended to be a practical tool to aid in the development of an effective biosafety program for laboratory workers. It promotes best laboratory practices to protect workers from exposure to infectious diseases encountered inside the laboratory and to minimize the potential transfer of infectious organisms outside the laboratory. OSHA requirements that apply to laboratories are covered throughout this document.
According to Christopher, the document describes practices that include, but are not limited to, the use of standard precautions, good laboratory practices (eg, disinfection of contaminated work surfaces), safety devices, personal protective equipment, and appropriate decontamination and disposal of biological hazards. Topics include safe transport of infectious substances, laboratory equipment hazards, occupational health, incident response, planning for public health emergencies, and best practices for biosafety training and competency assessment. The guideline emphasizes that specific policies and procedures, along with appropriate training of personnel on consistent application of laboratory precautions during the performance of work tasks, are essential administrative controls for the prevention of laboratory-acquired infections.
Proper collection and handling of samples
Diagnostic blood samples are the most common type of biological specimens drawn and sent to laboratories for being analysis. CLSI safety standards established for specimen collection are critical to laboratories in two important ways. First, the accuracy of test results relies heavily on proper collection of patient samples. Second, laboratory personnel are protected from potential pathogens through established practices and procedures. Several CLSI guidelines pertaining to blood specimens are available including the following:
GP41—Collection of Diagnostic Venous Blood Specimens—Seventh Edition 3 provides descriptive procedures for the collection of diagnostic specimens by venipuncture, including line collections, blood culture collection, and venipuncture in children.
Special considerations for collections from vascular access devices, blood culture collection, and collections in isolation environments are included, as well as how to handle emergency situations. The FDA has evaluated and recognized this standard for use in satisfying a regulatory requirement.
GP42—Collection of Capillary Blood Specimens—Seventh Edition4 provides procedures for collection of capillary blood specimens that contribute to the accuracy of the results and the safety of the patient and the healthcare professional. If done incorrectly, a simple capillary blood procedure can result in inaccurate results or even patient harm. Specifications for collection sites, puncture depth, and disposable devices used to collect, process, and transfer capillary blood specimens are addressed. GP42 also establishes requirements for single-use disposable devices for collecting, processing, and transferring capillary blood specimens, including those for point-of-care testing. The FDA has evaluated and recognized this standard for use in satisfying a regulatory requirement.
GP44-A4—Procedures for the Handling and Processing of Blood Specimens for Common Laboratory Tests; Approved Guideline—Fourth Edition5 considers multiple variables that are involved in handling and processing blood specimens. Its application should enable the user to recognize and control accuracy and precision factors that occur between the time of blood collection and the time of test performance. The guideline specifies criteria to assist the laboratory and health care practitioners in recognizing and reducing or eliminating preexamination errors resulting from improper handling of blood specimens.
Laboratory safety program
When lab directors, or supervisors, find themselves responsible for the creation and implementation of complete safety programs in their medical laboratories, CLSI standard GP17-A3—Clinical Laboratory Safety—3rd Edition6 contains general recommendations for implementing a high-quality laboratory safety program, which are provided in a framework that is adaptable within any laboratory. “This guideline includes aspects of a safety program, including maintenance and inspection, personal safety, and warning signs and labels. In addition, the guideline addresses fire prevention, electrical and radiation safety, and other potential laboratory hazards. Special considerations for anatomic pathology laboratories are also included. These recommendations can also form the basis for standards developed by accreditation organizations for laboratory accreditation,” said Christopher. Guidelines for specialized safety programs such as radiation safety, chemical hygiene, and bloodborne pathogens and biosafety are also included.
Conclusion
Per OSHA, more than 500,000 workers are employed in laboratories in the United States. The laboratory environment can be a hazardous place to work, and laboratory staff are exposed to numerous potential hazards including chemical, biological, physical, and radioactive hazards. Whether performing laboratory tasks within a large hospital setting or a small laboratory, lab safety is at the forefront of every task performed. CLSI standards set guidelines, a precedence that allows laboratorians to work with peace of mind that proper training is in place, that competency abounds, and that, if a matter arises, all involved understand the necessary procedures to ensure safety and mitigate damages.
References
- Medical Laboratory Observer, April 2022, https://www.mlo-online.com/home/article/21260861/2022-lab-of-the-year-runner-up-cincinnati-childrens-hospital-medical-center-clinical-laboratory.
- CLSI. Protection of laboratory workers from occupationally acquired infections; Approved guideline—Fourth Edition. CLSI document M29-A4. Wayne, PA: Clinical and Laboratory Standards Institute; 2014.
- CLSI. Collection of diagnostic venous blood specimens. Seventh ed. CLSI standard GP41. Wayne, PA: Clinical and Laboratory Standards Institute; 2017.
- CLSI. Collection of capillary blood specimens. Seventh ed. CLSI standard GP42. Clinical and Laboratory Standards Institute; 2020.
- CLSI. Procedures for the handling and processing of blood specimens for common laboratory tests; Approved guideline—Fourth Edition. CLSI document GP44-A4. Wayne, PA: Clinical and Laboratory Standards Institute; 2010.
- CLSI. Clinical laboratory safety; Approved guideline—Third Edition. CLSI document GP17-A3. Wayne, PA: Clinical and Laboratory Standards Institute; 2012.
CDC updates Monkeypox transmission questions and outlines lab safety guidelines for specimen handling
The Center for Disease Control and Prevention (CDC) released its response to questions regarding the transmission of Monkeypox in May 2022. CDC updated its lab safety guidelines after the virus was found in the United. States.
The Monkeypox virus is a completely different virus than the viruses that cause COVID-19 or measles. It is not known to linger in the air and is not transmitted during short periods of shared airspace. Monkeypox spreads through direct contact with body fluids or sores on the body of someone who has monkeypox, or with direct contact with materials that have touched body fluids or sores, such as clothing or linens. It may also spread through respiratory secretions when people have close, face-to-face contact.
In the current monkeypox outbreak, typically those who have contracted the disease have had close, sustained physical contact with other people who are infected with the virus. However, the CDC is continuing to study other possible modes of transmission, such as through semen.
Prior studies of monkeypox outbreaks show that spread of monkeypox virus by respiratory secretions appears uncommon. Most cases of monkeypox report close contact with an infectious person; however, it is unknown what role direct physical contact has versus the role of respiratory secretions. In instances where people who have monkeypox have travelled on airplanes, no known cases of monkeypox occurred in people seated around them, even on long international flights.
There are important differences between airborne transmission and transmission via respiratory secretions. Airborne transmission occurs when small viral particles become suspended in the air and can stay there for periods of time. These particles can spread on air currents, or sometimes even infect people who enter a room after the infected person has left. In contrast, monkeypox may be found in droplets like saliva or respiratory secretions that drop out of the air quickly. Long range (e.g., airborne) transmission of monkeypox has not been reported.
CDC currently recommends that people infected with monkeypox wear a mask if they must be around others in their homes if close, face-to-face contact is likely. In a healthcare setting, a patient with suspected or confirmed monkeypox infection should be placed in a single-person room; special air handling is not required. Any procedures likely to spread oral secretions (such as intubation and extubation) should be performed in an airborne infection isolation room.1
CDC established specimen collection guidelines for monkeypox virus. Laboratories with specimens that are suspected to contain monkeypox virus should contact their state or territorial public health department (contact list) or the CDC Emergency Operations Center (EOC) at 770-488-7100 for guidance. After consultation, laboratories can send appropriately collected specimens to their state or territorial public health laboratory for real-time polymerase chain reaction (PCR) testing.
Clinical laboratories should follow these guidelines when collecting specimens for monkeypox virus:
Collect at least two dry swabs from the same lesion.
Swab or brush lesion vigorously with two separate sterile dry swabs. Use a sterile nylon, polyester, or Dacron swab with a plastic, wood, or thin aluminum shaft. Do not use other types of swabs.
Place swabs in individual sterile containers. Do not add any transport media.
Refrigerate (2–8°C) or freeze (-20°C or lower) specimens within an hour after collection. Store refrigerated specimens for up to 7 days and frozen specimens for up to 60 days.
Send refrigerated specimens within 7 days of collection; ship frozen specimens within 60 days of collection. Specimens that are greater than 8°C upon receipt will be rejected. Ship on dry ice as category B.
Send both swabs to the state or territorial public health laboratory. All specimens should be sent through the state or territorial public health department, unless authorized to send them directly to CDC.
A state public health laboratory may test one of the paired dry swabs for presumptive results. CDC can provide monkeypox virus-specific testing on the second dry swab specimen if the first dry swab is non-variola orthopoxvirus positive at the state or territorial public health laboratory.2
CDC publishes non-variola orthopoxvirus PCR testing procedure update
The CDC Laboratory Outreach Communication System (LOCS) issued a Laboratory Advisory about the CDC’s real-time PCR test procedure to detect non-variola Orthopoxvirus.3
On May 30, 2022, the CDC published a real-time PCR test procedure to detect non-variola Orthopoxvirus. This procedure is intended for international partners and any laboratories interested in pursuing a laboratory developed test (LDT). This procedure includes sequence information for primer and probe development and cycling conditions.
This assay is designed to detect non-variola orthopoxviruses, including monkeypox virus. It is not intended to specifically detect monkeypox virus or to differentiate monkeypox virus from the other orthopoxviruses this assay detects. Clinical presentation and positive test results from a non-variola Orthopoxvirus assay is adequate for treatment and laboratories should notify the appropriate state or territorial public health authorities of positive results.
Public health laboratories have capacity for the current testing demand. Laboratories with specimens that are suspected to contain monkeypox virus should contact their state or territorial public health department as soon as possible.
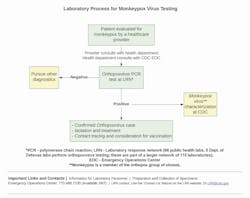
The CDC has advised that labs refer to the CDC Specimen Collection Guidelines for Monkeypox Virus for more information.4 (Also see Figure 1.)
References
- CDC Monkeypox Response: Transmission https://www.cdc.gov/media/releases/2022/0509-monkeypox-transmission.html (Accessed June 11, 2022).
- Lab Advisory: CDC Specimen Collection Guidelines for Monkeypox Virus https://www.cdc.gov/csels/dls/locs/2022/05-16-2022-lab-advisory-CDC_Specimen_Collection_Guidelines_Monkeypox_Virus.html? (Accessed June 11, 2022).
- Lab Advisory: CLARIFICATION – CDC Publishes Non-variola Orthopoxvirus PCR Testing Procedure https://www.cdc.gov/csels/dls/locs/2022/06-02-2022-lab-advisory-CLARIFICATION-CDC_Publishes_Non-variola_Orthopoxvirus_PCR_Testing_Procedure_1.html (Accessed June 11, 2022).
- CDC Laboratory Process for Monkeypox Virus Testing. https://www.cdc.gov/csels/dls/locs/2022/05-16-2022-lab-advisory-CDC_Specimen_Collection_Guidelines_Monkeypox_Virus.html? (Accessed June 11, 2022).
Gail Castanho, Managing Editor, MLO