“I think it’s just an allergy.” Almost every clinician hears that from patients, especially during allergy season. Many people believe that allergies explain their upper respiratory tract symptoms, such as cough, congestion, and runny nose. In fact, studies suggest that about 30 percent of Americans have allergies based on serum or skin test allergy results, and higher rates have been reported. However, it is important to recognize that many people with positive allergy tests do not have persistent respiratory symptoms and the true prevalence of allergic respiratory disease is less than commonly perceived.
Because many allergy symptoms mimic other health concerns, it is important for treating clinicians to understand the cause of these symptoms and whether or not their patient has true allergies or is suffering from some other condition. Colds and sinus disease, for example, share many clinical features with allergic rhinitis. While the symptoms can be similar, clinical details often identify patients with allergies. For instance, compared to other conditions, allergies far more commonly cause eye symptoms and an itchy, as well as runny, nose. Also worth noting, allergies do not cause fever.
The time of year can also be a clue: In many areas of the United States, pollen allergies begin in early spring and last until fall due to the pollination from trees, grasses, and weeds. However, wet but mild winter temperatures can cause plants to pollinate early in the spring or mold spores to be a problem during the winter months.
It is also important to note that some allergy sufferers may present with symptoms all year long, which may be the result of indoor allergens, such as mold, dust mites, or pet dander. Generally, these patients will have their worst symptoms when indoors at home or work, and in particular upon waking. If not pollen-sensitized, they may also report that their symptoms are less severe when outside.
The problem of self-diagnosis
Because allergies and upper respiratory infections (URIs) are prevalent, share symptoms, and are generally non-life threatening, it is not surprising that patients may be inclined to self-diagnose and over-diagnose one or both of these conditions. That’s a potential concern, because the treatments for allergies and URIs differ, and a patient may spend precious time and money on over-the-counter treatments that are appropriate for one condition but not the other.
Of greater concern than that: sometimes symptoms suggestive of allergic upper respiratory disease (or a simple cold) are actually due to more serious lower respiratory tract conditions such as asthma, influenza, or bacterial pneumonia. These can be particularly serious health conditions for some patients including the very young, the elderly, and patients with weakened immune systems. Moreover, some respiratory infections are easily spread, so proper diagnosis is vital to protect others from infection.
Asthma and allergies
Asthma is a lung disease sometimes confused with allergic upper airway disease (also known as allergic rhinitis or allergic rhino-sinusitis), and these conditions often coexist in the same patient. One study,1 based on analyses of 14 million IgE laboratory test results, found that people with positive IgE results for respiratory allergens are more likely to have asthma than those with negative results. Moreover, the study confirmed previous observations in noting that young children with food allergies commonly go on to develop respiratory allergies and asthma more often than young children who do not develop food allergies.
Because allergies are common and readily treatable, medical evaluation of patients with presumed respiratory allergy symptoms is important. In many cases, a medical evaluation will include the use of allergy testing to help confirm or exclude the allergy diagnosis. Positive results help physician and patient develop an effective allergy treatment plan, which may include environmental controls to reduce allergen exposure and/or medications. However, negative allergy results are equally useful, because they will lead to additional diagnostic investigation and an alternative diagnosis.
Laboratory allergy testing
Physicians may use skin prick tests or immunoglobulin E (IgE) blood tests to aid in the diagnosis of respiratory allergies, and these two approaches are generally considered to be equally reliable. However, only allergy specialists are trained to conduct allergy skin tests, while serum IgE tests are available to all healthcare providers through laboratory diagnostics. Moreover, while allergy skin testing takes about 20 to 30 minutes to complete, serum IgE testing only requires a small volume of blood.
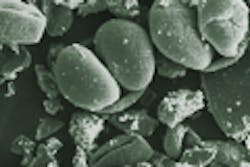
Immunoglobulin E (IgE) is an antibody that binds to the surface of mast cells and basophils through a special receptor called the high affinity IgE receptor. When these IgE armed cells encounter their allergen in the airways, they immediately release histamine and other substances that give rise to patient symptoms, including sneezing, congestion, and watery and itchy nose and eyes. However, while serum IgE tests help determine what allergens people are sensitized to, it is important to point out that many sensitized individuals will not develop symptoms after appropriate allergen exposure. For this and several other reasons, it is important that serum IgE allergy testing be evaluated in the context of a comprehensive medical evaluation by a practitioner well versed in the diagnosis and management of allergic diseases.
IgE technology is available for hundreds of individual respiratory allergens. Respiratory allergen panels are also customized, as it were, for multiple regions in the United States. Each includes allergens most prevalent in that region, making those panels ideal for diagnosing respiratory allergies.
Treatment steps post-diagnosis
While over-the-counter allergy medications are readily available, they are often misused by people suffering from respiratory symptoms not caused by allergies, as well as by allergic patients who are unaware of the best therapeutic strategies for their condition. Therefore, the most important first step in the management of allergies remains the clinical evaluation. This evaluation is likely to include allergy testing.
The good news for patients suffering from allergic upper airway diseases (allergic rhinitis, allergic rhino-sinusitis, and allergic rhino-conjunctivitis): many safe and effective therapies are available for the control of symptoms. These include environmental controls to reduce exposure to relevant aeroallergens based on allergy test results, antihistamines to control intermittent eye and/or nose symptoms, nasal steroids for chronic symptoms, and immunotherapy, which involves a series of injections with allergens to which a patient is known to be allergic. However, only with a good history, physical exam, and respiratory allergen testing results can a medical provider make a fully informed decision about how best to manage patients with allergic upper-airway disease.
REFERENCE
- Kaufman HW, Odeh MA, Bost WH, Ragothama P. Allergies across America: the largest study of allergy testing in the United States. Quest Diagnostics, Madison, NJ: 2011.
Anthony Horner, MD, certified by the American Board of Allergy and Immunology, serves as Associate Medical Director, Immunology for Quest Diagnostics. Quest provides a range of testing services to aid the diagnosis of allergies based on ImmunoCAP and other technologies.