Each day more than 200 patients die in the United States from infections they acquire while in a healthcare facility.1 These healthcare-associated infections (HAIs) are a major cause of morbidity and mortality, and are the fourth-leading cause of death in the U.S., resulting in more deaths than breast cancer and prostate cancer combined. In addition to the human cost, these infections cost the healthcare system between $28.4 billion and $33.8 billion a year.2 (These are 2009 estimates.)
HAIs can be acquired through invasive treatments such as surgery, indwelling medical devices including bloodstream, endotracheal, and urinary catheters, contact with a contaminated healthcare provider’s hands or environmental surfaces, and the overuse or improper use of antibiotics. The majority of healthcare-acquired HAIs include urinary tract infections, surgical site infections, bloodstream infections, and pneumonia. Catheter-associated urinary tract infections are among the most common; central line-associated bloodstream infections are potentially the most serious and life-threatening.
Exploring the problem
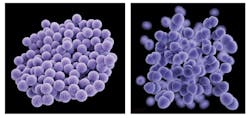
Many HAIs are due to organisms that are resistant to one or more of the most commonly prescribed antibiotics, and in some cases are resistant to all available drugs. These include methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), and multidrug-resistant Gram-negative bacteria (MDR-GNB). Patients infected with these multidrug-resistant organisms (MDROs) typically have increased mortality, increased hospital length of stay, and higher hospital costs than patients infected with susceptible organisms. This is due both to the delay in detecting MDROs and the subsequent delay in patients receiving adequate therapy, as well as the limited antibiotic treatment options that are now available for the most resistant infections.
To combat this serious problem, organizations including the United States Centers for Disease Control and Prevention (CDC) and the Society for Healthcare Epidemiology of America (SHEA) have developed evidence-based infection control guidelines to help prevent and reduce HAIs. In 2009, the National Action Plan to Prevent Health Care Associated Infections set five-year goals for the 25 percent to 50 percent reduction of various types of HAIs. The National and State Healthcare-Associated Infections Progress Report released by the CDC in March 2014 reported significant decreases in central line-associated bloodstream infections (44%) and surgical procedure-related infections (20%) between 2008 and 2012. It also reported minimal decreases in hospital-onset MRSA (4%) and Clostridium difficile (2%) infections, and an increase in catheter-associated urinary tract infections (3%).
Numerous publications have documented the efficacy of various combinations of infection-control measures including improved hand hygiene, contact precautions, active surveillance cultures, education, improved environmental cleaning, and improved communication measures to reduce the burden of MRSA, VRE, and MDR-GNBs at individual institutions. The results of the HAI Progress Report, however, indicate there is still much more work to be done on a national basis, and infection control measures are only a partial solution.
Current diagnostic methods
Early detection and diagnosis of infections is critical to ensuring patients receive effective therapy as early as possible, which will help prevent the emergence and spread of MDROs. Rapid diagnostic technologies such as peptide nucleic acid-based fluorescence in situ hybridization (PNA FISH), polymerase chain reaction (PCR), and mass spectrometry (MS) allow for the early identification of causative pathogens. These methods can identify microbial pathogens and resistance markers within a couple of hours, compared to conventional culture-based methods which can take up to one to two days for organism identification and two to four days for antibiotic susceptibility results.
The PNA FISH assays require a fluorescence microscope and can identify a limited number of organisms in 20 minutes following a Gram stain. Various PCR-based methods can identify Gram-positive, Gram-negative, and/or yeast organisms. These systems can also detect selected resistance markers such as mecA for MRSA detection, vanA/vanB for VRE detection, and various beta-lactam and carbapenem-resistance genes including CTX-M, IMP, KPC, NDM, OXA, and VIM found in Gram-negative bacteria in one to two hours or less from positive blood cultures and respiratory and wound samples.
More recently, matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF) MS instruments can identify organisms in minutes from isolated colonies, although off-label direct-from-sample procedures have been reported as well. These technologies have made important strides in demonstrating the value of rapid microbiology information by providing results to clinicians faster than conventional culture-based methods.
However, rapid microbial identification is only part of the answer. The results allow clinicians to modify empiric therapy earlier, but erring on the side of caution still can lead them to prescribe overly broad and often unnecessary therapy, which can perpetuate and exacerbate the MDRO problem.
Resistance marker results also deliver partial answers to clinicians. While the presence of resistance markers can provide insight into which antibiotic(s) to avoid, existing assays test only for a limited number of resistance genes and therefore cannot be used to safely narrow and optimize therapy for most organisms. In addition, even when resistance marker results are available, some clinicians do not know how to interpret the results, and end up waiting the two to four days for the conventional antibiotic susceptibility test results anyway.
Spotlighting new approaches
The next generation of rapid diagnostics will soon hit the market and provide even faster and much more comprehensive solutions for addressing HAIs and MDROs in hospital patients. These include miniaturized magnetic resonance (T2MR) and polymerase chain reaction/electrospray ionization mass spectrometry (PCR/ESI-MS) for direct-from-sample organism identification, and more recently multiplexed automated digital microscopy for both rapid pathogen identification and high-speed antibiotic susceptibility testing. T2MR uses coated nanoparticles to bind to target DNA in a sample and enhance the corresponding change in magnetic resonance signal for organism detection. The technology enables a 10- to 100-fold increase in sensitivity over PCR-based methods, allowing for detection of organisms directly from whole blood. Currently, a T2Candida test panel is available for the identification of five Candida species directly from blood and is designed to produce results in as little as three to four hours.Another technology uses PCR to amplify microbial nucleic acid and ESI-MS to determine the nucleic acid base composition of the pathogen(s), and then compares this composition to a database for microbial identification. Recently CE marked, this platform can detect hundreds of bacteria and Candida species, as well as four antibiotic resistance markers (mecA, vanA, vanB, and KPC) directly from EDTA whole blood, sterile fluid, or tissue samples in approximately eight hours.
Another solution that is currently under development is multiplexed automated digital microscopy, which provides both rapid microbial identification and faster time-to-antibiotic susceptibility results. The automated, sample-to-answer system uses FISH for identification of 19 bacterial and yeast targets within one hour, and time-lapse imaging of surface-immobilized bacterial cells in the presence of antibiotics to measure the growth response and generate antibiotic susceptibility results from a panel of 30 antibiotics in another four hours. This platform delivers minimum inhibitory concentration (MIC) and susceptible-intermediate-resistant (SIR) results directly from samples such as positive blood cultures and respiratory specimens within five hours. Given clinicians’ familiarity with antibiotic susceptibility results, the system could provide a more comprehensive and effective solution for early optimization of antibiotic therapy.
References
- Magill SS, Edwards JR, Bamberg W, et.al. Multistate point-prevalence survey of healthcare associated infections. NEJM. 2014;370:1198-1208.
- Division of Healthcare Quality Promotion, National Center for Preparedness, Detection, and Control of Infectious Diseases, Coordinating Center for Infectious Diseases, Centers for Disease Control and Prevention. The Direct Medical Costs of Healthcare-associated Infections in U.S. Hospitals and the Benefits of Prevention. www.cdc.gov/hai/pdfs/hai/scott_costpaper.pdf. Accessed December 26, 2014.