Do you think there’s “nothing new under the sun” with regard to urinalysis? Until recently, that may have been the case. Urinalysis, the world’s oldest diagnostic test, was long regarded in the laboratory as a necessary, labor-intensive procedure which provided invaluable but limited information for clinicians. Now, however, urinalysis is changing, courtesy of a new generation of analyzers that integrate and automate its two primary functions: chemistry and microscopic particle analysis. Technological advances are opening the door for the introduction of new renal biomarkers which will revolutionize diagnosis of acute tubular necrosis (ATN) in the same way that cardiac biomarkers revolutionized diagnosis of cardiac disease. As the aging population continues to stress healthcare systems, it becomes paramount to understand the implications of these technological breakthroughs in the urinalysis lab.
Hippocrates (460-377 B.C.) was the first to mention bubbles in urine as a diagnostic tool for kidney disease and “long illness,”1 but using the appearance and odor of urine to diagnose disease goes back farther than that. There has been a steady progression in the sophistication of uroscopy, or urinalysis by the senses, through the millennia: from ancient Hindus noting that black ants were attracted to sweet urine, to the medieval development of the graduated urine glass known as a matula for determining color; from the first qualitative urine glucose test in 1850, to automated dipstick readers in the 1970s; from Leeuwenhoek’s single lens microscope in 1595, to the urine particle flow cytometers of today. What has remained constant through this evolution is the need for skilled labor to successfully identify diagnostic issues. And as the pool of skilled talent in the laboratory has continued to shrink in recent years, the need for integration, automation, and rapid identification has increased.
A potent tool
Urinalysis remains a potent screening tool for the clinician. It is still, as Simerville and colleagues noted, “invaluable…in the diagnosis of urologic conditions such as calculi, urinary tract infection, and malignancy” and “the presence of systemic disease affecting the kidneys.”2 No other laboratory test can provide as much information on the status of metabolic, renal, infectious, and urologic functions in the body. As a result, physicians use UA for everything from general screening to cancer detection. While test strip technology is what usually comes to mind when one thinks of urinalysis, microscopic examination is a necessary partner. Chemistry alone cannot detect casts, crystals, cells, and bacteria, which are critical for early diagnosis of many disease states. Indeed, in an era when failure to quickly detect hospital-acquired infections such as catheter-associated urinary tract infections (CAUTIs) means the loss of significant revenue to a hospital, the need to integrate urine chemistry testing with urine particle analysis is paramount.
Further, the need for greater accuracy is driving movement from manual methods of the past to the automation solutions that are available today. Due to inaccuracies inherent in manual methods, they are not precise enough to capture rare but clinically significant elements.3 Automation solves many of the issues that beset the traditional manual methods, including discrepancies in sample volume, urine drop size, aged samples, and cellular breakdown. Most important, it addresses the labor issues inherent in any manual method; in addition to the matters of sample handling and technologist time, it avoids the issue of subjective judgment. Minimizing human error that occurs when technologists read a test strip or scan an image is a key to quality results.
The key to early detection
Several emerging categories of disease may warrant the combined power of urine chemistry and cellular analysis reports. While reflex testing is available on most automated platforms, there are a number of situations in which a urine chemistry panel will be normal, so the reflexive particle exam will not occur. However, the cells and particles may hold the key to early detection by physicians of situations that constitute sentinel events for a hospital or individual patient. Three such situations are UTI screening and detection, early renal disease detection, and bladder cancer.
• UTIs: Urinary tract infections are a significant exposure for hospitals on multiple levels. There is a need for rapid screening for outpatients admitted through the ER, particularly patients from skilled nursing facilities. If a patient is admitted with documentation of an existing UTI, then there is less risk of suspicion that the infection may be hospital-acquired. Such screening mandates a rapid and sensitive method to detect bacteria, something urine cultures and urine chemistries alone cannot provide. Urine cultures take 24 to 48 hours; urine chemistry cannot detect all bacteria, leaving only cellular analysis to detect all bacteria quickly—but manual procedures cannot cope with the quantity of tests such screening would entail. The only option is fully automated urine particle analyzers.
Further aggravating the situation, hospital acquired CAUTIs, considered sentinel events, have grown to approximately 450,000 per year in the U.S., adding an average of $1,000 to the care of each patient.4 The total financial impact on U.S. hospitals is $450 million. The financial risk to hospitals is that payors may not cover costs for hospital-acquired infections. Automated platforms can report the actual number of bacteria in urine with a level of specificity and sensitivity that is unmatched by manual and image-based systems. Integrated platforms ensure that the cells are counted within minutes of the chemistry strip testing, providing a comprehensive report within STAT turnaround time goals. With early detection and intervention of CAUTIs, hospitals can manage their risk and financial exposure.
• Renal disease: With diabetes on the rise, affecting 8.3% of the U.S. population, the need for early detection of renal impairment that can lead to chronic kidney disease is critical. According to the National Diabetes Information Clearinghouse 25.8 million people are affected; of those, seven million are undiagnosed. In 2010, 27% of U.S. residents over 65 had diabetes. The total cost for diabetes in 2007 was $174 billion, with medical expenses for diabetics twice that of non-diabetics.5 Kidney disease, however, can be managed with early detection. In addition to creatinine and µALB, accurate detection of microhematuria (rare or few RBC) through cellular analysis can be critical for physicians.
Even more critically, acute kidney injury (AKI) and the associated acute tubular nephropathy (ATN) can lead to imminent kidney failure and death. The traditional methods of supporting physician assessment of kidney function, BUN and creatinine, have significant disadvantages: for instance, it takes about 24 hours for the creatinine level to rise, even if both kidneys have ceased to function. Alternative markers have been proposed (such as NGAL, KIM-1, IL18, and cystatin C), but none currently replaces creatinine as a marker of renal function. Urine cell analysis is the only alternative at present. Writes the Mayo Clinic’s Lieske: “Urinalysis is a very helpful test for identifying evidence of kidney damage. Ordinarily there are very few formed elements in urine. However, after acute kidney injury, renal epithelial cells (REC) can be shed into the tubular lumen and detected in the urine.”6 Red blood cells (indicating glomerular inflammation or breakdown), white blood cells (infection), REC casts, and granular casts can be quantified in low levels with automated urine particle analyzers.
• Bladder Cancer: One of the earliest tests to detect bladder cancer is detection of RBC in urine sediment. The American Urological Association guidelines indicate that clinically significant microhematuria is ≥3 RBC/hpf (40x) from two to three properly collected urine samples; however microhematuria can range from 1 to10 RBC/hpf, depending on the patient’s risk factors.7 Manual microscopy reports results in “bins,” such as “0-3/hpf,” which may lead to uncertainty in physician interpretation. Is a result that falls in the “0-3 RBC/hpf” bin a true 0, a 1, or a 3/hpf? Is this result positive or negative for the risk factors of the individual patient? If you have a result of 2 RBC/hpf, it could be interpreted by physicians as a positive risk factor for bladder cancer if the patient is a smoker. The ability to quantify low end RBC/hpf for physicians may be critical to catching this disease early, when treatment is most successful. Only automated urine particle analyzers have the level of sensitivity and specificity needed to differentiate at low levels.
Considering the space issue
In the cost and space-conscious laboratory, urinalysis workstations tend to be compact by necessity. It can be difficult to carve out the space needed for multiple stations, which can lead to difficult choices. Rather than eagerly embracing the new integrated, automated platforms available, many labs stick with manual methods, missing out on opportunities to significantly reduce labor and turnaround time and increase the accuracy of results. All three of these directly and indirectly drive total cost; any decision to evaluate urinalysis systems must include a value calculation for these costs.
Many labs conclude that the benefit of upgrading a urinalysis workstation will offset the space required. Moreover, there are new systems looming on the horizon which will truly “do more with less”—less space. These integrated platforms require half the bench space of older platforms.
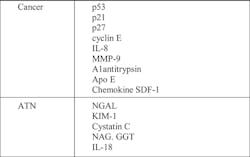
There is also the potential for new biomarkers for ATN, such as NGAL and KIM-1, and urologic cancers (Table 1) along with more traditional urine chemistry tests such as creatinine and µALB to be added to routine urinalysis.
Urinalysis has a dynamic future. New technology for instrumentation, new biomarkers, and new appreciation for the importance of urinalysis in modern medicine are combining to bring the focus back to where laboratory testing started so long ago—while also bringing urinalysis into the 21st century.
References
- White WL. A new look at the role of urinalysis in the history of diagnostic medicine, Clin Chem. 1991;37:119-125.
- Simerville JA, Maxted WC, Pahira JJ. Urinalysis: a comprehensive review. Amer Fam Phys. 2005;71(6):1153-1162.
- Dotson M. An examination of urine microscopic sediment analysis. Sysmex J Int. 2001;11:40-42.
- Fuchs MA, Sexton DJ, Thornlow DK, Champagne MT. Evaluation of an evidence-based, nurse-driven checklist to prevent hospital-acquired catheter-associated urinary tract infections in intensive care units. J Nurs Care Qual. 2011;26(2):101-109.
- National Diabetes Information Clearinghouse. http://diabetes.niddk.nih.gov/dm/pubs/statistics/. Accessed July 23, 2013.
- Lieske JC. Biomarkers of acute renal failure. Mayo Medical Laboratories’ Hot Topics. August 2009. http://www.mayomedicallaboratories.com/articles/hottopics/transcripts/2009/2009-8b-renal-failure/8b-6.html. Accessed July 23, 2013.
- Cohen RA, Brown RS. Clinical practice. Microscopic hematuria. N Engl J Med. 2003;348:2330–2338.