Improving liver disease outcomes: four decades of advances in diagnostics technology
During the last four decades, advances in science have resulted in remarkable achievements in combating hepatitis. This is attributable to translational research discoveries in immunology and genetics that allowed the development of sophisticated diagnostics technologies that made the blood supply safe and helped physicians diagnose and treat hepatitis more effectively.
Translational research, according to the Journal of the American Medical Association, refers to “bench to bedside” science that applies basic knowledge and new discoveries to produce drugs, medical devices, diagnostics, and other clinical tools.1 The outcome is the creation of new approaches and technologies for prevention, diagnosis, and treatment of disease. There is no better example of the benefits accrued from translational research than the more than 40-year legacy of technological advances in diagnosing and monitoring viral hepatitis.
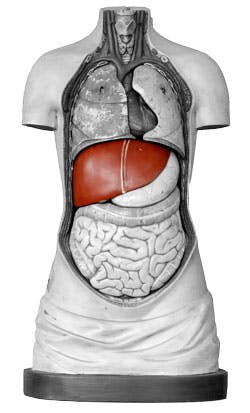
The overall health of the liver
Weighing about three pounds, the liver is the second largest organ in the body. It is involved in processing everything we eat and drink and converting it to energy and nutrients, while also filtering harmful toxins from the bloodstream. To check liver function, physicians order liver enzyme tests as part of routine physical examinations. These tests are performed in almost every laboratory on high-volume clinical chemistry analyzers and measure levels of ALT, AST, ALP, and GGT. Elevated levels of any of these enzymes can be a sign of liver or bile duct damage. Abnormal results of liver enzyme tests may lead to further testing to determine if the patient has possible liver damage caused by HBV or HCV.
The term hepatitis indicates inflammation of the liver. A hepatitis infection can be brief and self-limiting or may present a chronic condition, with the liver being inflamed for many weeks, months or years. Hepatitis often occurs with few or no symptoms, while in other cases the disease can produce jaundice, malaise, and loss of appetite. Most hepatitis cases worldwide are caused by a group of hepatitis viruses. Other causes include toxins, including alcohol, and certain medications, as well as autoimmune diseases.
In addition to the liver enzyme tests, more specific tests may be required to determine the etiology of a possible hepatitis case. They include assays to check for an immune response to a hepatitis virus or to determine if the virus is present in the serum of the person presenting with hepatitis. Such tests can detect viral proteins in the serum of an infected person or identify viral genetic material (DNA or RNA) in serum.
Immunoassays: the first breakthrough
In the early 1970s, virologists made significant discoveries identifying and classifying hepatitis viruses and isolating specific antibodies and antigens that could be used as diagnostic probes to find these viruses in blood. The first commercial so-called sandwich immunoassay for detection of the hepatitis B surface antigen was introduced in 1972, and a test for hepatitis A soon followed. Through the 1970s and 1980s, several more assays were developed to measure different serological markers for hepatitis A and B. As a result, physicians were empowered to accurately stage and monitor the infections. For HBV, a panel of diagnostic markers can help determine if the patient has an acute infection, is an asymptomatic chronic carrier, or is capable of passing the disease to others. For hepatitis A (HAV), the presence of IgM class antibodies against the virus is an indicator of acute infection.
Even though the immunoassays for HAV andHBV were a major leap forward in managing liver disease, a type of hepatitis aptly called non-A, non-B hepatitis was still a threat. The discovery of HCV in 1989 led to an immunoassay for detection of anti-HCV antibodies in blood donor screening and patient diagnosis.
With all of these advancements, a variety of tests are available worldwide to ensure a safe blood supply and to diagnose viral hepatitis. Blood screening is performed to identify donors who may transmit hepatitis virusesto transfusion recipients. Serology testing for hepatitis B surface antigen (HBsAg), molecular testing for the presence of HBV DNA, and HCV testing (antibody tests for HCV, and in many areas HCV RNA testing) are used in blood bank laboratories worldwide.Some countries perform a test to detect antibodies to the HBV core protein as an additional measure to prevent HBV infection from donors who may be infected with HBV but may test negative for HBsAg or HBV DNA.
Also, there is increasing concern about two other hepatitis viruses, HAV and HEV, which usually are self-limiting and appear transiently in blood. At a recent Blood Products Advisory Committee meeting, the potential threat of hepatitis E Virus (HEV)-contaminated blood was addressed, along with a proposal for studies to determine if the blood supply in the United States should be screened for HEV.2 In some countries, testing for HEV has become more important as increasing numbers of cases are being recognized in geographic areas where HEV was not believed to be prevalent.
For patient diagnosis, serology tests for HAV, HBV, and HCV may be supplemented with molecular-based tests to determine if the person is actively infected with these viruses or whether they have resolved infection. Alternatively, the HBsAg and HCV core antigen tests can be utilized to distinguish whether a person is actively infectedor is resolving the infection.
Molecular diagnostics advances
Today, molecular diagnostics offers laboratories of all sizes the ability to provide earlier and more accurate detection of hepatitis, thanks to automated instrument systems utilizing polymerase chain reaction (PCR) and other molecular technologies to identify and measure viral RNA. Further simplification of molecular assays and instruments is expected to foster wider implementation by community hospital laboratories.
Scientists have identified the genes and mutations responsible for replication of hepatitis viruses. Their discoveries are being explored by researchers striving to design molecules that interfere with enzymes and other viral-encoded molecules required for viral replication.
As new hepatitis treatments emerge, precise diagnostics technologies are essential for monitoring therapy.These results help physicians determine whether to begin antiviral therapy, influence decisions on dosing and therapy duration, and identify drug resistant strains.
Monitoring antiviral therapy
Genotyping is a process of classifying viruses into related groups based on the similarity of their genetic material. Hepatitis viral genotype testing may aid in the recommended regimen for antiviral therapy because some hepatitis viral genotypes are more responsive to antiviral drugs than others. In its clinical practice guideline published in 2011 in Hepatology, the American Association for the Study of Liver Diseases recommended that HCV genotyping should be performed in all HCV-infected persons prior to interferon-based treatments in order to plan for the dose and duration therapy and to estimate the likelihood of response.3 The viral load assays that are utilized to monitor antiviral therapy must provide accurate measurement of viruses from all the genotypes that occur in infected patients.
For HCV monitoring, a widely used molecular assay can detect and accurately quantitate HCV RNA genotypes 1 through 6. The HCV viral load tests can determine if the individual has had a sustained viral response, which in most cases indicates the patient no longer is infected with HCV, or whether treatment has been only partly effective or ineffective. Alternatively, HCV core antigen testing has been utilized in some cases to monitor the efficacy of antiviral therapy.
An HBV molecular assay introduced in the U.S. in 2009 covers all known HBV genotypes (A-H) by targeting an essential, highly conserved segment of the HBV genome. All eight HBV genotypes are found in the United States. As with HCV, the HBV DNA viral load test can be utilized to monitor antiviral therapy. With the emergence of new antiviral compounds, there are increasing numbers of individuals whose serum is free from circulating virus, as indicated by the absence of detectable HBV DNA. However, in many cases, the livers of these individuals continue to harbor HBV, as shown by continued presence of viral proteins (e.g., HBsAg) in their serum and the presence of HBV DNA in liver tissue. So in order to determine the status of patients with this profile, there is continued need for HBsAg testing for monitoring antiviral therapy.
Genetic sequencing
Beyond viral loads and genotyping, genetic sequencing tests for HBV and HCV can measure changes in the viral genome associated with drug resistance. Gene sequencing tests are used in tandem with viral load and genotyping assays to monitor drug treatments and determine if unexpected elevations in viral loads are caused by drug-resistant mutations. After assessing viral load and genotyping results, a physician may decide to order a sequencing test to choose or change antiviral therapies based on the known drug resistance profile of a specific hepatitis virus.
Genetics will exert even greater influence on the diagnosis and treatment of hepatitis and other infectious diseases in the near future. A new genetic marker, the Interleukin 28B gene, (IL28B), can predict sustained viral response to interferon-based treatment for HCV. Published studies have shown that a genetic polymorphism near the IL28B gene is associated with a two-fold change in response to interferon-ribavirin treatment for HCV. IL28B, therefore, could help stratify patients for HCV treatment.4
We are at the early stages of applying genomics to understand risk genes for liver disease and identifying patients most likely to respond to various treatments. Another area of research, termed proteomics, is also being applied to better understand risk for liver disease.Proteomics involves the exhaustive analysis of protein structure and function in an organ or tissue. In clinical proteomics, levels of gene expression are often compared between diseased and non-diseased tissue to determine if there is a qualitative or quantitative difference in protein markers. Proteomics is being applied to liver disease, with hope that markers will emerge for early detection of hepatocellular carcinoma, early or more accurate diagnosis of autoimmune hepatitis, and for non-alcoholic fatty liver disease (NAFLD). Other future markers could foster more accurate diagnosis of liver fibrosis progression and serve as prognostic indicators for chronic infection with HBV and HCV.
Already we have seen growing acceptance of molecular testing for hepatitis diagnosis and monitoring. Soon it might be used more routinely and earlier than called for by current testing algorithms. History has shown that translational research in immunology and genetics has fostered new diagnostic technologies, and that process will continue and result in even greater achievements for combating liver disease.
REFERENCES
- Woolf SH. The meaning of translational research and why it matters. AMA. 2008;299:211-213.
- Issue Summary, Blood Products Advisory Committee, 104th Meeting. September 20, 2012. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/BloodVaccinesandOtherBiologics/BloodProductsAdvisoryCommittee/UCM319542.pdf Accessed February 7, 2013.
- Ghany MG, Nelson DR, Strader DB, Thomas DL, Seeff LB. An update on the treatment of Genotype 1 chronic hepatitis C virus infection: 2011 Practice Guideline by American Association for the Study of Liver Diseases. Hepatology. 54:1433-1444. doi:10.1002/hep.24641.
- Kempuraj D, Donelan J, Frydas S, et al. Interleukin-28 and 29 (IL-28 and IL-29): new cytokines with anti-viral activities. Int Immunopathol Pharmacol. 17(2):103-106.