PSA results and lab changes, disinfectant for blood alcohols, Staph aureus and haemophilus workups, and selection of antibiotic disk
Comparing PSA results when changing labs
Q: We have a patient who has been
getting PSA tests from another lab. When he had a test in our lab, the values showed a considerable increase. The doctor wants to know if this is a real increase in PSA, or if it is only due to the fact that the values are from two different labs. What should we do?
A: Longitudinal measurements for
following a tumor marker must use a test system that does not change during the course of time. This is true of PSA as well as for CEA for colon cancer surgery follow-up, beta-2-microglobulin for multiple myeloma, or HCG for testicular carcinoma or choriocarcinoma. For that matter, the same problem occurs when an anticoagulated patient having serial prothrombin times changes laboratories.
Whenever there is a method or reagent system change in testing a patient who is being followed by serial measurements, an overlap between the two methods must be done, otherwise it is impossible to know whether a result change was due to a change in the patient or the method. In the case of the patient in this question, I would recommend that the physician arrange for the patient to have at least one, and preferably more, crossover tests performed by both the old and new laboratories simultaneously. This could be accomplished by having a single blood sample drawn, split, and sent to both labs. The physician can then compare the simultaneously obtained values to see if there was a change. It is not safe to rely on comparing the test result with the reference ranges for the two labs because for PSA, there are significant differences between methods in regard to standardization and the sensitivities to free versus total PSA.
Daniel M. Baer, M.D.
Professor Emeritus
Department of Pathology
Oregon Health and Science University
Portland, OR
Disinfectant for blood alcohols
Q: I have a question about the
ethanol assay. Our assay literature says that we shouldnt use an alcohol disinfectant. Would this really affect the assay, since our alcohol wipe pads contain isopropyl alcohol?
A: You are correct to question the
cross-reactivity of isopropyl alcohol with an assay that measures ethyl alcohol (ETOH). Studies have shown that when high concentrations of isopropyl alcohol are added to an ethanol-free serum pool, some cross-reactivity occurs, at least for colorimetric assays.1 However, there is no evidence I am aware of that documents that an ETOH level will be significantly altered when performed on a specimen collected from a site cleansed with the standard isopropyl alcohol pad. Its always best to follow manufacturers guidelines, and I would ultimately refer you to the assays manufacturer as to the rationale behind the recommendation in the product literature.
Regardless of the lack of documented evidence, the concern is for how a judge or jury, typically not well-versed in laboratory technology, will perceive the accuracy of the results. To most attorneys, the case is significantly weakened if the results of the test can be called into question. Justifiable or not, blood alcohol levels drawn from sites prepped with alcohol cast doubt upon the outcome in the eyes of lay judges and jurists. All the jury needs to acquit is reasonable doubt, and that can be easily placed before a jury of laypeople by an attorney who can show that isopropyl alcohol cross-reacts in any way, regardless of the practical application of the evidence. Therefore, all specimens to be tested for alcohol should be drawn from a site cleansed with nonalcohol-based skin cleansers.2
Dennis J. Ernst MT(ASCP)
Center for Phlebotomy Education Inc.
Ramsey, IN
References
- Vitros Test Methodology: Alcohol [package insert]. Raritan, NJ: Ortho-Clinical Diagnostics; 1996.
- National Committee for Clinical Laboratory Standards. Procedures for the Collection of Diagnostic Blood Specimens by Venipuncture. Approved standard H3-A4. Villanova, PA; 1998.
Staph aureus and haemophilus workups
Staphylococcus aureus recovered from throat and expectorated sputum cultures always considered clinically significant, regardless of the quantity present?
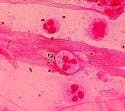
A: The interpretation of culture
results on throat and expectorated sputum is difficult because the upper respiratory tract may be colonized with potential pathogens (e.g., H.influenzae, Staphylococcus aureus, Streptococcus pneumoniae, Enterobacteriaceae) that are not involved with the infection. Because these agents are often recovered on the culture medium, the laboratory should develop a procedure that minimizes over-reporting of these bacteria.
The interpretation of throat cultures is less complicated than sputum cultures because viruses cause most cases of pharyngitis, and the primary cause of bacterial pharyngitis is Streptococcus pyogenes.3 Although H. influenzae, S.aureus, and S. pneumoniae are frequently isolated from throat cultures, they have not been shown to cause pharyngitis and are not reported.4 Other bacterial agents that occasionally cause pharyngitis and are reported when recovered include group B and C beta-hemolytic streptococci, Neisseria gonorrhoeae, Arcanobacterium haemolyticum, Corynebacterium diphtheriae, Chlamydia pneumoniae, and Mycoplasma
spp.
Source: Gloria J. Delisle, Lewis Tomalty, authors. Licensed for use, ASMMicrobeLibrary
(www.microbelibrary.org)
David Sewell, Ph.D., ABMM
Director of Microbiology,
Veterans Affairs Medical Center
Portland, OR
References
- Barlett JG, Ryan KJ, Smith TF, Wilson WR, Washington JA II. Laboratory diagnosis of lower respiratory tract infections. In: Cumitech 7A. Washington, DC: American Society for Microbiology; 1987:1-18.
- James L, Hoppe-Bauer JE. Processing and interpretation of lower tract specimens. In: Isenberg HD, ed. Clinical Microbiology Procedures Handbook. Washington, DC: American Society for Microbiology; 1992:1.15.1-1.15.8.
- Gwaltney JM, Bisno A. Pharyngitis. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases. 5th ed. 2000:656-662.
- Forbes BA, Sahm DF, Weissfeld AS. Upper respiratory tract infections and other infections of the oral cavity and neck. In: Bailey & Scotts Diagnostic Microbiology. 10th ed. 1998:321-328.
Selection of antibiotic disk
Q: hospital where the physicians ask the laboratory to test each newly approved antimicrobial agent. This practice results in setting up two susceptibility plates for each organism tested. Currently, we test one representative disk for each class of antimicrobial agents on the hospitals formulary. How do we address this problem?
A: Clinicians rely on the clinical
microbiology laboratory for assistance in the selection of appropriate therapy for patient care because the susceptibility of organisms to antimicrobial agents is not always predictable. However, this does not mean that the laboratory must test every available antimicrobial agent. The selection of a battery of antimicrobial agents for testing is difficult and must consider a number of factors, including clinical efficacy, cost, prevalence of resistance, minimizing emergence of resistance, acceptable in vitro test performance for selected organisms, and current consensus recommendations. The laboratory can, in some cases, minimize the number of agents selected by testing one drug that can be used to predict the activity of a class of agents; not testing all comparable drugs that yield similar interpretive results and clinical efficacy; and not testing agents with predictable results. Annually, the NCCLS publishes an excellent document that addresses these issues and lists the antimicrobial agents that should be tested and reported for each group of organisms, or tested and reported selectively; alternative agents that may be useful for resistant or unusual organisms; and agents that should be tested only on organisms isolated from urine.1 Because the selection of an appropriate battery of antimicrobial agents to test and report is based on complex issues, the decision should be made in consultation with the infectious disease clinicians and the pharmacy and therapeutics committee of the medical staff.
David Sewell, Ph.D., ABMM
REFERENCE
- Performance Standards for Antimicrobial Susceptibility Testing: 11th Informational Supplement. Wayne, PA: NCCLS; 2001. M100-S11.
Daniel M. Baer is professor emeritus of laboratory medicine at Oregon Health and Science University in Portland, OR, and a member of MLOs editorial advisory board.
December 2002: Vol. 34, No. 12
©
2002 Nelson Publishing, Inc. All rights reserved.