T cells from common colds cross-protect against infection with SARS-CoV-2
People with higher levels of T cells from common cold coronaviruses are less likely to become infected with SARS-CoV-2, according to a news release from Imperial College London describing a new study.
The study, published in Nature Communications and led by Imperial College London researchers, provides the first evidence of a protective role for these T cells. While previous studies have shown that T cells induced by other coronaviruses can recognize SARS-CoV-2, the new study examines, for the first time, how the presence of these T cells at the time of SARS-CoV-2 exposure influences whether someone becomes infected.
The researchers also say their findings provide a blueprint for a second-generation, universal vaccine that could prevent infection from current the time of SARS-CoV-2 exposure influences whether someone becomes infected.
Rhia Kundu, first author of the study, from Imperial’s National Heart and Lund Institute, says, “Being exposed to the SARS-CoV-2 virus doesn’t always result in infection, and we’ve been keen to understand why. We found that high levels of pre-existing T cells, created by the body when infected with other human coronaviruses like the common cold, can protect against COVID-19 infection.”
The study began in September 2020 when most people in the UK had neither been infected nor vaccinated against SARS-CoV-2. It included 52 people who lived with someone with PCR-confirmed SARS-CoV-2 infection and who had, therefore, been exposed to the virus. The participants did PCR tests at the outset and 4 and 7 days later, to determine if they developed an infection.
Blood samples from the 52 participants were taken within 1-6 days of their exposure to the virus. This enabled the researchers to analyze the levels of pre-existing T cells induced by previous common cold coronavirus infections that also cross-recognize proteins of the SARS-CoV-2 virus.
People with higher levels of T cells from common cold coronaviruses are less likely to become infected with SARS-CoV-2.
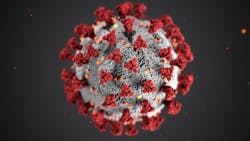
The researchers found that there were significantly higher levels of these cross-reactive T cells in the 26 people who did not become infected, compared to the 26 people who did become infected. These T cells targeted internal proteins within the SARS-CoV-2 virus, rather than the spike protein on the surface of the virus, to protect against infection.
Current vaccines do not induce an immune response to these internal proteins. The researchers say that — alongside our existing effective spike protein-targeting vaccines — these internal proteins offer a new vaccine target that could provide long-lasting protection because T cell responses persist longer than antibody responses which wane.