The entire healthcare community is painfully aware of the impact that the COVID-19 pandemic has had on patients, staff, healthcare facilities, capacity, and supplies. The effect on laboratories has been two-fold. First, the shutdown of many essential and non-essential services and procedures had a direct impact on general laboratory testing volumes, putting many businesses in a very difficult position financially. Second, the demand for new testing to support the needs of COVID-19 diagnosis and treatment had laboratories that were forward-thinking, scrambling to retrofit their equipment, reagents, test supplies, and operations to support the demand. While this had a positive financial impact for those facilities, it also directly impacted their resources to support their standard test menus and processes.
Oncology was one of the medical service lines impacted by the pandemic. The pandemic — including the shutdown of all non-essential services — has had a devastating impact on oncology screening, testing, biopsies, surgeries, diagnosis, and treatment for patients in the United States. The long-term effects are as yet unknown, but certain presumptions can be made based upon the data.
For a person who has new symptoms, or needs to begin the screening process, the impact has been catastrophic. A survey of 356 cancer centers in 54 counties detailed the impact of the pandemic on the delivery of cancer services. The majority of centers (88%) said they had reduced the level of care. More than half said the reductions were precautionary, but others noted other reasons, such as an overwhelmed system (20%), staff shortages (18%), and lack of access to medications (10%)1.
When asked about the potential harm to patients from the service disruptions, 46% said more than 10% of patients missed at least one chemotherapy session.1
Authors of another paper noted declines in new cancer diagnoses in the United States. In a research letter in JAMA Network Open, they analyzed de-identified data on diagnostic testing for eight cancer types from January 2018 to March 2021, based on 799,496 patients. After dividing the data into three pandemic periods (March-May 2020, June-October 2020, and November 2020-March 2021), they found a significant decline in new diagnoses of cancer in the first and third pandemic periods but not the second period.2
These numbers are daunting if you look at the potential impact that decreases and delays in diagnosis and treatment can have for an oncology patient. The situation can literally have a direct impact on their prognosis.
For example, in a study in The Lancet Oncology, researchers said that delays in diagnosis and treatment are expected to be associated with increases in mortality in the United Kingdom from breast, colorectal, and lung cancers by as much as 9.6%, 16.6%, and 5.3%, respectively, up to 5 years after diagnosis.2 The authors attributed the delays to COVID-19 pandemic mitigation measures, such as lockdowns.3
How can we as a community and a profession do better? What options and solutions are available to prevent these types of disruptions, as surges in the COVID-19 pandemic occur for an unforeseen period of time? Is there anything we can do to neutralize some of the damage that has already been caused to oncology patients by these initial delays in screening, diagnosis, and treatment?
The rise of digital pathology
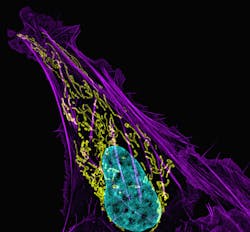
Digital pathology became a relevant response to safely provide access to pathologists anytime and anywhere. Digital pathology efficiently reduces the time to diagnosis and provides pathologists with access to patient case information by delivering the whole slide images electronically and in an automated, integrated environment. This helps the pathologist by providing all of the information that they need to diagnose a patient quickly and accurately, then enables the instantaneous distribution of that information back to the ordering clinician.
Efficiency gains have been seen in the 20-40% range, based upon studies done by labs that have implemented the technology.
To facilitate the use of digital pathology during the pandemic, the U.S. Food and Drug Administration (FDA) issued a temporary order in April 2020, relaxing the requirements for the use of remote-reviewing and reporting of scanned digital images and pathology slides.4
The policy is in place for the duration of the pandemic, and the agency may decide to make it permanent.
The goal of the policy is to allow laboratories and pathologists to diagnose patients remotely using digital pathology and AI-assisted technologies, following specific validation processes. In the guidance, the FDA said it would not object to the alteration or modification of FDA-cleared devices or the marketing of new pathology devices for remote use.
Providing fast, timely diagnosis for a patient, and being able to send the report automatically and instantaneously to their ordering physician or oncologist, will enable patients to get into treatment plans much faster.
A relatively small number of laboratories were using digital pathology prior to the pandemic. These laboratories were able to scale their use and provide support to patients and physicians, while others realized the benefits of putting an operational plan in place to adopt digital pathology. The ability to have real-time access to patient information and pathologists, who may be working from other locations outside the lab, quickly became a prime consideration.
Laboratories that use digital pathology solutions will also be able to minimize any impact that a resurgence in COVID-19, such as the one we are currently seeing with the Delta variant, will have on the continued care for oncology patients. Implementing digital solutions now also will help labs cope with future pandemics and other states of emergency that could negatively impact the pathology workflow.
The entire workflow of the patient case (whole slide images, interpretation, and diagnosis) can all be done safely from any location when a complete, secure, and remotely accessible solution is in place. This, in addition to all the known and expected benefits of deploying digital pathology and AI solutions, is a compelling reason for healthcare entities to expedite their plans for including digital workflows in their operations in the near term. It has become obvious that planning for unforeseen events that are as negatively impactful as this pandemic is necessary, yet always 20/20 in hindsight. Lessons learned show us that being prepared, based on our current knowledge and experience, can ensure that patients, especially oncology patients, can continue to receive the screening and diagnostic healthcare that they need in a timely manner.
Artificial intelligence
Artificial intelligence (AI) algorithms are a sure way to gain ground on some of the time lost for patients by assisting pathologists in speeding up the time to diagnosis. AI algorithms for varying applications are readily available and are being developed in an increasing number of content areas. There are algorithms that can help identify abnormal cells, identify specific types of tumors, and triage cases higher in the work queue of pathologists, based upon the interpretation of a higher potential risk for positivity or complexity. Algorithms also perform mundane tasks, such as counting cells and performing calculations to determine cancer scores and severity grading. All of these are excellent tools for a pathologist to leverage, adding efficiencies that facilitate faster patient diagnosis and with greater confidence.
It is clear why the focus of technological advancements in pathology are on digital pathology, AI and image analysis, as they support a faster diagnosis and increase accuracy when combined with the professional expertise of a pathologist. As digital pathology becomes more widely adopted, we can hope for faster diagnoses, more prevalent application of personalized, targeted treatment, and better outcomes for the patient. The ability to diagnose patients while supporting the need for quarantines or social distancing among professionals who are in remote locations is a great added bonus for healthcare facilities and patients alike.
References
- Jazieh A, Akbulut H, Curigliano G, et al. Impact of the COVID_19 pandemic on Cancer Care: A collaborative study. JCO Glob Oncol. 2020 Sep;6:1428-1438. doi: 10.1200/GO.20.00351.
- Kaufman H, Chen Z, Niles J, Fesko Y. Changes in newly identified cancer among US patients from before COVID-19 through the first full year of the pandemic. JAMA Netw Open. 2021 Aug 2;4(8):e2125681.doi: 10.1001/jamanetworkopen.2021.25681
- Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: A national, population-based modelling study. Lancet Oncol. 21:1023—1034. 2020.
- U.S. Food and Drug Administration. Enforcement Policy for Remote Digital Pathology Devices During the Coronavirus Disease 2019 (COVID19) Public Health Emergency. Guidance for Industry, Clinical Laboratories, Healthcare Facilities, Pathologists, and Food and Drug Administration Staff. https://www.fda.gov/media/137307/download. April 2020. Accessed September 8, 2021.
About the Author

Lisa-Jean Clifford
Lisa-Jean Clifford has been a noteworthy leader in the high-tech healthcare solutions space for more than two decades. Lisa-Jean’s passion for making a positive impact on the lives of patients through technology can be traced back to her tenure at McKesson and IDX, now GE Healthcare, where she served in vital business development and marketing roles, and to Psyche Systems, an LIS solution provider, where she was the CEO for eleven years. She is currently the President at Gestalt Diagnostics.
Now, recognized as an industry expert, she actively participates in numerous boards including the Association of Pathology Informatics where she serves as President and MLO’s Editorial Advisory Board. She is widely published in many top laboratory publications and noteworthy news sources, such as Forbes, CAPToday, Medical Laboratory Observer, and Health Data Management. Also, she is a highly sought-after speaker and focuses on delivering valuable content in critical areas such as lab automation including software and interoperability, digital pathology, AI in pathology, lab informatics, oncology, and women’s health.