Transfusion medicine at Moffitt Cancer Center focuses on best practices
Transfusion medicine is an important part of the treatment process for many cancer patients, whose disease and treatment might lead to bleeding or clotting issues, too few red blood cells, or other hematologic issues.
Benson, who has been at Moffitt since 1989, completed a fellowhship earlier in her career at the American Red Cross Blood Services in Los Angeles, where she also served as Assistant Medical Director.
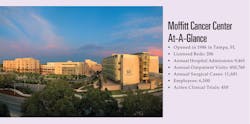
Since it opened its doors in 1986, Moffitt Cancer Center has treated patients from every state and many countries.
When is a red blood cell (RBC) transfusion clinically indicated for cancer patients?
Our indications for cancer patients are similar to other patient populations in that we transfuse for hemodynamically unstable, acutely bleeding patients; transfuse for symptomatic anemia with hemoglobin <8 g/dL; transfuse for acute myocardial ischemia with hemoglobin <9 g/dL; and will consider transfusion in asymptomatic patients who have hemoglobin <7 g/dL, although it may be unnecessary in a stable patient, especially those with chronic anemia.
We ask that single-unit RBC transfusion is considered first, in contrast to the outdated double-unit transfusion minimum of the past. We do use a transfusion threshold of <9 g/dL for patients prior to photopheresis or peripheral blood stem cell collection and higher thresholds may also be used for patients with unique needs such as in sickle cell anemia patients with prior stroke.
Approximately what percentage of Moffitt’s transfusions are with RBC units?
In 2019, we transfused 15,699 RBC units and performed 11,621 platelet transfusions, so you can see that 57 percent of our cellular components transfused are RBCs and 43 percent are platelets. Another way to look at it is that 1.4 RBC units are transfused for every platelet transfusion.
When it comes to transfusion medicine in oncology, what are some new developments in the science of RBC transfusions that are being incorporated into best practices at Moffitt?
Many have adopted the phrase “less is more” as we now have several studies showing that restrictive transfusion practices using lower hemoglobin thresholds may work as well or better than more liberal transfusion practices using higher thresholds. We have also found that for many patients, we do not have to transfuse the traditional two units of RBCs, and that many otherwise stable patients may do quite well with single units of blood when there is an indication for RBC transfusion.
Why does Moffitt routinely use irradiated blood in its transfusions?
Irradiated cellular blood components (RBCs and platelets) are routinely provided to our oncology patients since many patients have a clear need due to risks for transfusion-associated graft-versus-host disease (GVHD), such as recipients of blood and marrow transplantation or patients with hematologic malignancies. As we have an irradiator onsite, we have found it best to have an inventory of irradiated cellular components that are readily available should any of our patients in need require these components quickly. While other patient diagnoses may be at less risk for transfusion-associated GVHD, we have decided to err on the side of caution and transfuse these irradiated components to our oncology population.
When are plasma transfusions medically indicated in cancer care?
Some prime examples are patients with thrombotic thrombocytopenic purpura (TTP) who require fresh frozen plasma (FFP) for their therapy that includes plasma exchange. Some of our patients may have coagulation factor depletion during severe infections, disseminated intravascular coagulation (DIC), or bleeding and may require plasma transfusions at that time.
When are platelet transfusions medically indicated in cancer care?
Oncology patients often have low platelet counts due to their disease preventing them from making sufficient quantities of their own platelets, or due to our therapies like chemotherapy, or BMT, which can cause a temporary suppression of the patient’s platelet production. Also, patients with active bleeding can deplete their platelets and may require platelet transfusion along with the RBCs and plasma, which are typically needed in hemorrhaging patients.
What are new developments in the use of plasma and platelet transfusions in cancer care?
Fortunately, the three patients that had this low-risk event in Moffitt’s 30-plus years of operation did all fully recover but all occurred in smaller-sized patients who were non-group O receiving group O platelet transfusion. Based on these cases, we established a new mitigation step of plasma volume reduction of group O platelets to be transfused to smaller (less than 60 kg) non-group O recipients.
Will you explain the science behind Intercept-screened platelets and why some cancer centers choose to use these platelets for transfusions? Does Moffitt use these types of platelets?
Intercept platelets are apheresis platelets exposed to the psoralen amotosalen, which will bind to any nucleic acids present in the sample. Upon exposure to UVA light, crosslinking of the nucleic acids occurs, thus, preventing pathogen replication. The Intercept method has been shown to inactivate a broad range of pathogens, most importantly bacteria but also viruses, parasites, spirochetes and leukocytes. As bacterially contaminated platelets remain one of our chief concerns due to the high morbidity and potential mortality of these events, we have been eager to use PRT platelets and are slowly ramping up our inventory of this preferred component.
What advancements are on the on the horizon for reducing pathogens in blood products?
Currently here in the United States, we have pathogen reduction technology (PRT) platelets but do not yet have PRT RBCs. Methods for PRT RBCs have been developed and clinical trials have begun. With the PRT method, we may be able to ultimately discontinue some of the donor testing that we currently employ. We may be able to allow deferred donors to return to blood donation and possibly relax some of our donor restrictions.
What other steps can pathologists take to reduce the risk of adverse events associated with transfusions?
We can educate our medical colleagues to use evidence-based medicine when transfusing patients, educate our nursing colleagues to ensure proper patient- and blood-component identification at the time of transfusion, encourage patients’ loved ones to consider blood donation to replenish this limited resource, and serve as a ready source of guidance when questions arise.
Has Moffitt noted shortages in the supply of blood products as a result of the pandemic and people’s reluctance to donate blood?
Fortunately, our new blood suppliers – LifeSouth Community Blood Centers and SunCoast Blood Centers – have done an excellent job of keeping an adequate supply of blood on our shelves. In the past, we have experienced some shortages, generally over holidays and summer months. We did develop a blood shortage action plan due to the pandemic but, thankfully, have not had to implement it to date.
Moffitt signed agreements with both LifeSouth Community Blood Centers and SunCoast Blood Centers earlier this year. How have these agreements improved Moffitt’s access to blood? How had Moffitt been sourcing blood before signing the agreements?
Prior to signing these agreements, we had used OneBlood as our sole blood supplier. OneBlood and the former Florida Blood Services (and their predecessor Southwest Florida Blood Bank) had been our sole supplier since Moffitt first opened its doors back in 1986. We made the transition from a single supplier to a dual system in hopes of ensuring a consistent and adequate supply of blood. We hope that the adage “two are better than one” applies in this case.