At-home genetic-testing kits for breast and ovarian cancer risk are just as effective, and in some cases even more so, than the typical protocol for genetic testing, which requires repeated office visits and counseling, according to a study led by UW Medicine researchers.
The results, published this month by the American Society of Clinical Oncology (ASCO), found no increased stress after genetic testing for women who did not receive pre- and post-test counseling and who received only electronic education in the three-year study called MAGENTA, or Making GENetic Testing Accessible.
Dr. Elizabeth Swisher, a UW Medicine specialist in gynecologic oncology and one of the lead authors, expressed surprise at the finding that personalized telephone counseling—in which a subject could talk with a genetics expert before and after being tested—was not necessary. “Patients had no increased anxiety or stress if they skipped that counseling process and just received online genetic education," she said.
The results strongly indicate that at-home testing is a viable option for women to find out whether they have a propensity for these cancers, said Swisher. Her research and clinical focuses on cancer genetics and on the prevention, early detection, and treatment of ovarian cancer. The results also support making individualized genetic counseling available only to patients with positive test results, the report concluded.
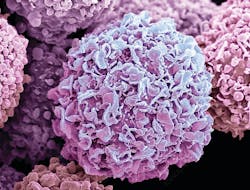
The study screened for BRCA1 or BRCA2 gene mutations, indicating a higher risk of breast cancer. It also tested for thousands of mutations in 17 other genes that increase the risk of breast and/or ovarian cancer. Among the 3,822 participants, those with the lowest response rate were in the study arm that included counseling before testing. The testing process was more often completed by women who did not have to undergo pre-test counseling.
The report involved input from researchers at MD Anderson, the Mayo Clinic, Memorial Sloan Kettering Cancer Center, and the Dana Farber Cancer Institute. The three-year MAGENTA trial finished enrolling participants in December. MAGENTA provided a free home genetic test for women who were at risk for ovarian cancer by dint of family history or who had had breast cancer but not received genetic testing. The study recently concluded the first three-month follow-up of participants; 12- and 24-month checkups will follow. The participants included women from all 50 states.
One main goal of the study was to discern whether the requisite patient experience for genetic testing—an office visit, counseling, blood draws, and then another visit—might be a barrier to participation. The study found that this was indeed the case. The next steps will be to analyze outreach to underserved groups: those living in rural areas, who are not Caucasian, and/or did not have a college degree. Among the study subjects, 90 percent were white and/or highly educated.