Integrate your point-of-care testing for gains in cost savings, staff productivity, & patient care
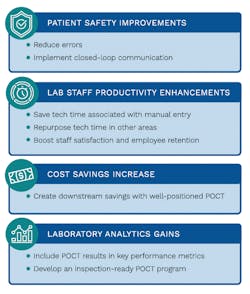
Point-of-care (POC) testing, in the appropriate patient care scenarios, provides significant benefits to patient care. The biggest advantage to POC testing is that by providing faster access to test results, diagnosis and subsequent treatment is expedited. However, to harness that rapid turnaround time (TAT), results must be captured at the point of care and made immediately available to the caregivers responsible for taking action based on those results.
POC testing growth spurred by the pandemic
Prior to the COVID-19 pandemic, POC testing was already experiencing significant growth and broader acceptance. With a renewed focus on improving population health at more affordable costs, the case for POC testing is strong, especially in situations where a quick TAT can have a profound impact on downstream costs and patient outcomes.
With the pandemic came a greater recognition of the value of POC testing and the importance of rapid test results along with an increased demand for reliable testing methodologies. Vendors are responding to this demand with improved methodologies and interfaceable devices, which are also driving adoption.
Benefits of data capture at the POC
Because POC testing sites can be widely scattered across a healthcare campus, it is important to have a robust POC testing management system to capture important test information and manage regulatory compliance.2 Ideally, the POC testing program can be efficiently and effectively monitored from a remote location.
Few healthcare organizations have been able to successfully integrate their POC test results into their Laboratory Information System (LIS) and Electronic Health Record (EHR). Decentralization of POC testing makes connectivity more challenging and contributes to the fact that only 10% of POC test results are electronically integrated.3 The full value of POC testing is only seen when those results are immediately accessible in the patient’s EHR.
Opportunity for significant time & money savings
As a primary benefit to the laboratory, capturing POC results at the testing location can save laboratory professionals a significant amount of time when compared to the time it takes to manually type results into the LIS or EHR. Time saved translates into cost savings and efficiency improvements for the entire organization. Below are two examples of integrated POC testing saving technologists’ time:
- Integrated bedside glucose improves lab productivity
Prior to integrating their bedside glucose testing, a healthcare organization in Nebraska was manually entering thousands of bedside glucose results. Laboratory staff were spending a significant amount of time writing down results at the bedside, traveling to the lab to manually enter results, and performing the required verification of those manually entered results.
Implementing a connectivity solution eliminated inefficiencies and errors associated with manual entry. Their laboratory saved more than 700 hours annually that staff can now use to focus on other tasks. With this example, the potential savings within a large healthcare facility add up to a substantial amount. For instance, a conservative estimate of annual bedside glucose testing volume in a large teaching hospital approaches $70,000 per year.4 If each glucose takes one minute to manually enter, this is equivalent to 1,167 hours of staff time; multiplied by an average Medical Assistant (MA) hourly wage of $18 per hour,5 this equates to about $21,000 per year spent in labor costs associated with the manual entry of bedside glucose testing. Calculated using the average Medical Laboratory Scientist (MLS) hourly wage of $36 per hour, it equates to more than $42,000 per year attributed to typing in glucose results.
- POC testing connectivity saves more than 3,300 hours of tech time
Prior to implementing a connectivity solution, POC testing operators at a large hospital in Ohio were manually typing results into the EHR or scanning instrument printouts for urinalysis (UA) testing. On average, manually entering results took 2.5 minutes because a UA contains ten or more components to enter; therefore, for every 24 UAs, entering results took an hour of tech time. To put this in perspective, their UA volume is approximately 80,000 per year, adding up to 3,333 hours spent manually entering results for that one lab test. Using the average MA wage for entering results, this means that their laboratory spent nearly $60,000 in one year in staff time allocated to this task alone.
In addition, to avoid the labor-intensive method of manually ordering and entering UA results, some of their testing locations were scanning the UA analyzer printouts or hand-written manual log sheets into the EHR because it was easier and faster. In this scenario, data mining for those test results is impossible because there is no discrete data. With a connectivity solution, the lab was able to eliminate this error-prone workflow and gain the efficiencies brought on by a comprehensive POC testing management and connectivity solution.
Patient safety boon
When results are not captured at the time of testing, the opportunity for errors and mishandling of test results increases. There is always the concern that caregivers and providers are not receiving results in a timely manner. Optimizing your organization’s health information technology capabilities so that closed-loop communication is in place, via automated ordering and reporting of POC test results, helps ensure patient safety and improves patient outcomes.
Connectivity standards are improving POC testing data capture
Two decades ago, there was no electronic data management for POC testing; results were manually recorded in paper charts or on log sheets in the testing area. To improve connectivity for POC testing, in 2000, the Connectivity Industry Consortium developed POC testing connectivity standards that have since evolved into the Clinical and Laboratory Standards Institute (CLSI) POCT1-A. In 2005, the POCT1-A standard was upgraded to POCT-01-A2. The standard’s purpose is to standardize POC test connectivity so that devices are easily interfaced to information systems. CLSI now has a consensus committee that oversees the development of ongoing POC testing standards.
Today, many devices can reduce or eliminate operator and analytical errors, and POC testing management systems are available that enable automatic electronic flow of data from the devices to the LIS and EHR, as well as provide remote access to quality control (QC) and operator certification data.
POCT must be integrated to reach full potential
Having a strong POC testing management system and connectivity solution can dramatically reduce the amount of time spent typing in results, eliminate errors inherent to manually entered results, and facilitate real-time access to results so that providers can make timely care decisions.
When POC test results are captured at the time of testing, valuable savings in tech time are achieved, freeing staff to perform other tasks. Automatically capturing results through POC testing also provides tools that improve employee job satisfaction because laboratory professionals realize that their time and expertise are better used outside of manual result entry. Furthermore, having a closed-loop communication where the order is placed electronically and results transmit back into that system as soon as they are available reduces errors associated with manual entry and that, in turn, improves patient safety.
In the advancing arena of healthcare data analytics to support patient-centered care and population health management, it is no longer a luxury to have POC testing electronically integrated—it is a necessity. POC testing must be immediately available in the patient’s chart so that the benefits associated with rapid TAT are fully realized, and the POC test data is included in the overall data snapshot of the healthcare organization to facilitate analytics-driven business decisions.
References
- Park KS, Heo H, Choi YK. Design and realization of integrated management system for data interoperability between point-of-care testing equipment and hospital information system. Healthcare Informatics Research. 2013;19(3):222–228. doi: 10.4258/hir.2013.19.3.222
- Lewandrowski K, Gregory K, Macmillan D. Assuring quality in point-of-care testing: Evolution of technologies, informatics, and program management. Archives of Pathology & Laboratory Medicine. 2011;135(11),1405-1414. doi: 10.5858/arpa.2011-0157-RA
- Blick KE. The essential role of information management in point-of-care/critical care testing. Clinica Chimica Acta. 2001;307(1-2),159-168. doi: 10.1016/s0009-8981(01)00460-0
- Lee-Lewandrowski E, Laposata M, Eschenbach K, et al. Utilization and cost analysis of bedside capillary glucose testing in a large teaching hospital: Implications for managing point of care testing. Journal of Medicine. 1994;97(3),222–230. doi: 10.1016/0002-9343(94)90004-3
- Medical Assistant Salary in the United States. Salary.com. Accessed at https://www.salary.com/research/salary/benchmark/medical-assistant-salary. Accessed May 4, 2022.
- Clinical Laboratory Scientist Salary in the United States. Salary.com. Accessed at https://www.salary.com/research/salary/listing/clinical-laboratory-scientist-salary. Accessed May 4, 2022.
Kim Futrell, MT (ASCP), MSHI Senior Strategic Marketing Manager, Orchard Software.
About the Author

Kim Futrell, MT (ASCP), MSHI
is the Products Marketing Manager at Orchard Software. Prior to joining Orchard in 2012, Futrell, who has a Master of Science in health informatics, worked as a lab manager for more than 20 years.