Neurofilament light chain: Unraveling the diagnostic and prognostic threads in neurological disorders
The pathological foundation of numerous acute and chronic neurological disorders, leading to enduring disability, lies in neuroaxonal damage and loss. The capability to easily identify and track such damage would offer significant advantages in evaluating disease activity, monitoring responses to treatment, and predicting prognosis. Neurofilaments are attracting growing interest as potential biomarkers for neuroaxonal injury. These abundant structural scaffolding proteins are exclusively present in neurons and show elevated levels in response to axonal damage in various conditions, including neurodegenerative, inflammatory, vascular, and traumatic diseases. Notably, this increase is observable not only in cerebrospinal fluid (CSF) but also in blood. The specificity of neurofilaments for neuronal cell damage and eventual cell death provides a distinct advantage over other potential biomarkers. Neurofilaments are proteins classified as type IV of intermediate filaments (including the three neurofilament proteins) and are exclusively expressed in the cytoplasm of neurons. Together with microfilament and microtubules, neurofilaments form the neuronal cytoskeleton. As of today, there are five known neurofilament subunits that can be differentiated by their molecular mass. Besides neurofilament light (NfL), medium (NfM), and heavy (NfH) with molecular masses of approximately 68, 150 and 200 kiloDalton (kDa), peripherin and internexin with a molecular mass of 57 and 66 kDa exist.1 While NfL, NfM, and NfH are ubiquitously expressed in mature neurons, internexin is mainly found in central nervous system while peripherin is in the peripheral nervous system. Due to their stability and role in the neuronal structure, they gained interest in usage as markers for axonal damage. As the intermediate filaments always contain NfL, it was determined to be the optimal molecule for use as a biomarker.2
Neurofilament light chain biomarkers: Which holds the diagnostic edge – blood or CSF?
Upon damage, neurofilaments leak into the interstitial space and eventually into CSF and blood (serum, plasma) where it can be quantified. While blood NfL concentration is at a lower level than CSF NfL concentration, there is a tight and strongly positive association between CSF NfL and blood NfL levels.3 CSF collections require lumbar punctures that are associated with more side effects such as headaches, backaches, nausea, or vomiting. In recent years, however, the development of improved assay technologies now allows for reliable NfL quantification in blood samples.4
How specific is neurofilament light chain as a clinical biomarker?
Any neuroaxonal damage or degeneration can lead to NfL release into the CSF and bloodstream. The clinical specificity of NfL as a biomarker can vary depending on the specific neurological disorder. It is crucial to emphasize that although increased levels of NfL are linked to neurodegeneration, they are not specific to a particular disease. In addition to increases due to clinical relapses in multiples sclerosis (MS), NfL levels can be influenced by age, comorbidities, and other diseases such as Alzheimer’s disease (AD), amyotrophic lateral sclerosis (ALS), Parkinson’s disease, as well as in stroke, traumatic brain injury (TBI), and epilepsy. Of these diseases, NfL is most strongly associated with MS.4 NfL appears to increase with age as well as show more variability. Studies have shown that NfL levels in the blood of healthy people can increase by 2.2% per year.5 These increases in the older population are likely partially explained by the higher prevalence of comorbidities such as diseases or stroke. Cardiovascular risk factors such as high body mass index (BMI), smoking and blood pressure, as well type 2 diabetes can also influence NfL levels, and careful interpretation is necessary in a clinical context.4
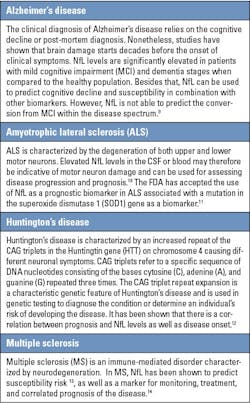
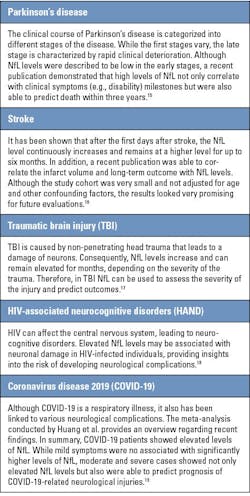
How does neurofilament light chain manifest across a spectrum of neurological disorders?
A recent publication analyzed blood NfL concentrations in 13 neurodegenerative diseases, Down syndrome, and depression.6 An increase in blood NfL levels was observed in all of them, confirming its role as a marker of neurodegeneration. Easy access to blood biomarkers such as NfL can play a significant role in the management of neurological disorders. It can be used as a rapid screening tool to identify or reject neurodegeneration as an underlying cause of cognitive symptoms for AD and beyond.7
Elevated NfL levels can also indicate non-disease-specific neuronal damage. Thus, interpretation of NfL results should always consider the overall clinical context and should be combined with a prior established disease diagnosis. Ongoing research continues exploring the utility of NfL as a biomarker in various neurological conditions, and its role in predicting risk and monitoring disease is continually evolving. A good overview regarding the use of NfL can be found in the review by Barro et al.7 and Khalil et al.8
Table 1 gives an overview of different diseases and the potential benefits for the use of NfL.
REFERENCES
1. Yuan A, Nixon RA. Neurofilament Proteins as Biomarkers to Monitor Neurological Diseases and the Efficacy of Therapies. Front Neurosci. 2021;27;15:689938. doi:10.3389/fnins.2021.689938.
2. Mücke N, Kämmerer L, Winheim S, et al. Assembly Kinetics of Vimentin Tetramers to Unit-Length Filaments: A Stopped-Flow Study. Biophys J. 2018;22;114(10):2408-2418. doi:10.1016/j.bpj.2018.04.032.
3. Disanto G, Barro C, Benkert P, et al. Serum Neurofilament light: A biomarker of neuronal damage in multiple sclerosis. Ann Neurol. 2017;81(6):857-870. doi:10.1002/ana.24954.
4. Khalil M, Teunissen CE, Otto M, et al. Neurofilaments as biomarkers in neurological disorders. Nat Rev Neurol. 2018;14(10):577-589. doi:10.1038/s41582-018-0058-z.
5. Thebault S, Booth RA, Freedman MS. Blood Neurofilament Light Chain: The Neurologist's Troponin? Biomedicines. 2020;21;8(11):523. doi:10.3390/biomedicines8110523.
6. Ashton NJ, Janelidze S, Al Khleifat A, et al. A multicentre validation study of the diagnostic value of plasma neurofilament light. Nat Commun. 2021;7;12(1):3400. doi:10.1038/s41467-021-23620-z.
7. Hampel H, O'Bryant SE, Molinuevo JL, et al. Blood-based biomarkers for Alzheimer disease: mapping the road to the clinic. Nat Rev Neurol. 2018;14(11):639-652. doi:10.1038/s41582-018-0079-7.
8. Barro C, Chitnis T, Weiner HL. Blood neurofilament light: a critical review of its application to neurologic disease. Ann Clin Transl Neurol. 2020;7(12):2508-2523. doi:10.1002/acn3.51234.
9. Jung Y, Damoiseaux JS. The potential of blood neurofilament light as a marker of neurodegeneration for Alzheimer's disease. Brain. 2024;4;147(1):12-25. doi:10.1093/brain/awad267.
10. Abu-Rumeileh S, Vacchiano V, Zenesini C, et al. Diagnostic-prognostic value and electrophysiological correlates of CSF biomarkers of neurodegeneration and neuroinflammation in amyotrophic lateral sclerosis. J Neurol. 2020;267(6):1699-1708. doi:10.1007/s00415-020-09761-z.
11. Benatar M, Wuu J, Andersen PM, et al. Design of a Randomized, Placebo-Controlled, Phase 3 Trial of Tofersen Initiated in Clinically Presymptomatic SOD1 Variant Carriers: the ATLAS Study. Neurotherapeutics. 2022;19(4):1248-1258. doi:10.1007/s13311-022-01237-4.
12. Byrne LM, Rodrigues FB, Blennow K, et al. Neurofilament light protein in blood as a potential biomarker of neurodegeneration in Huntington's disease: a retrospective cohort analysis. Lancet Neurol. 2017;16(8):601-609. doi:10.1016/S1474-4422(17)30124-2.
13. Bjornevik K, Munger KL, Cortese M, et al. Serum Neurofilament Light Chain Levels in Patients With Presymptomatic Multiple Sclerosis. JAMA Neurol. 2020;1;77(1):58-64. doi:10.1001/jamaneurol.2019.3238.
14. Abdelhak A, Benkert P, Schaedelin S, et al. Neurofilament Light Chain Elevation and Disability Progression in Multiple Sclerosis. JAMA Neurol. 2023;1;80(12):1317-1325. doi:10.1001/jamaneurol.2023.3997.
15. Frank A, Bendig J, Schnalke N, et al. Serum neurofilament indicates accelerated neurodegeneration and predicts mortality in late-stage Parkinson's disease. NPJ Parkinsons Dis. 2024;9;10(1):14. doi:10.1038/s41531-023-00605-x.
16. Ahn JW, Hwang J, Lee M, et al. Serum neurofilament light chain levels are correlated with the infarct volume in patients with acute ischemic stroke. Medicine (Baltimore). 2022;30;101(39):e30849. doi:10.1097/MD.0000000000030849.
17. Shahim P, Gren M, Liman V, et al. Serum neurofilament light protein predicts clinical outcome in traumatic brain injury. Sci Rep. 2016;7;6:36791. doi:10.1038/srep36791.
18. Hagberg L, Edén A, Zetterberg H, Price RW, Gisslén M. Blood biomarkers for HIV infection with focus on neurologic complications-A review. Acta Neurol Scand. 2022;146(1):56-60. doi:10.1111/ane.13629.
19. Huang Z, Haile K, Gedefaw L, et al. Blood Biomarkers as Prognostic Indicators for Neurological Injury in COVID-19 Patients: A Systematic Review and Meta-Analysis. Int J Mol Sci. 2023;30;24(21):15738. doi:10.3390/ijms242115738.
About the Author

Dr. Thomas Kampfrath, PhD, DABCC, NRCC
PhD, DABCC, NRCC
is a board-certified clinical chemist and medical officer for Siemens Healthineers.

Dr. Sascha Lange
Dr.
is a biochemist and serves as director of Clinical Sciences for Siemens Healthineers.