The ongoing troponin conundrum: Understanding an elevated troponin
As laboratory assays have evolved with improved performance, the clinical use of cardiac troponin (cTn) has also evolved beyond the context of myocardial infarction (MI). The release of high sensitivity (hs) cTn assays has led to even more changes in clinical and laboratory guidelines for cTn use and expanding data on additional clinical uses. As defined in the Fourth Universal Definition of Myocardial Infarction,1 “the clinical definition of MI denotes the presence of acute myocardial injury detected by abnormal cardiac biomarkers in the setting of evidence of acute myocardial ischaemia.” The preferred biomarkers for myocardial injury evaluation are cTnI and cTnT, with hs-cTn assays recommended for routine clinical use.1,2 Myocardial injury is defined by an elevated cTn value, with at least one value above the upper reference limit (URL), as defined by the 99th percentile of a health population. Therefore, MI is a type of myocardial injury, but not every myocardial injury is an MI.
With the advent of hs-cTn assays, as required to qualify an assay as being highly sensitive, now more than 50% of healthy individuals (>80% for some assays) will have a detectable troponin. Gone are the days when any detectable troponin was an indicator of a potential evolving health emergency or poor prognosis. Now, clinicians must be able to assess a troponin result in consideration of the many causes of troponin elevation and patterns over time. Clinical decisions for interpretating hs-cTn elevations, including potential use of rule-in/rule-out algorithms, make it critical to have accurate cTn results and to interpret the results in the context of the patient’s presentation, clinical history, and other assessments (e.g., ECG results). This high sensitivity in more healthy individuals brings a challenge of accommodating the differential diagnosis for different types of myocardial infarction and injury that release troponin into the blood, so as not to contribute to unnecessary work-ups and procedures. Data on risk stratification using cTn, including when below the 99th percentile URL, is being studied, to elucidate appropriate cutoffs and interpretation.
Across the continuum of myocardial injury
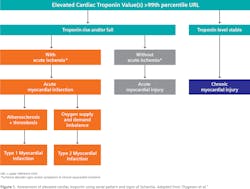
Serial testing of cTn in patients needing testing has grown in importance with the shift to hs-cTn assays, to help identify presence of an acute (rising and/or falling pattern) versus chronic elevation of cTn (see later section “Biological-related cardiac troponin elevations”). Additionally, there is an increased need to understand different clinical classifications of MI beyond the ST-segment elevation (STEMI), non-ST-elevation MI (NSTEMI), and unstable angina paradigm. More nuanced classifications describe various types of MI, based on their pathological, clinical, and prognostic differences along with associated differences in treatment strategy. The criteria for type 1 MI includes a rise and/or fall of cTn values with at least one value above the 99th percentile, and at least one related appropriate sign of artherothrombotic coronary artery disease (Figure 1).1 This “traditional” type of MI must be distinguished from another group of diseases that cause acute myocardial ischemia but due to another reason. Type 2 MI involves ischemic myocardial injury caused by an oxygen supply and demand mismatch, also requiring similar cTn criteria as type I with evidence of the mismatch from symptoms, imaging, or ECG changes. Some examples of type 2 MI include coronary embolism, hypotension or shock, and respiratory failure.
In the presence of a cTn above the 99th percentile URL, the serial troponin pattern helps distinguish acute versus chronic myocardial injury, and the presence or absence of signs and/or symptoms of clinical myocardial ischemia help further distinguish acute myocardial injury from acute myocardial infarction (type 1 versus type 2 MI; Figure 1). MI types 3, 4, and 5 involve cardiac death and coronary procedure–related ischemia, and more information can be found within the referenced publications.1Defining and interpreting an elevated troponin
Two overarching groups of elevated cTn in the absence of MI include causes related to 1) biological factors, including other disease states that can cause acute or chronic myocardial injury, and 2) assay factors, including interferences and pre-analytical influences. A contributing effect may begin with a choice made prior to even beginning use of a cTn assay, when making the choice of the 99th percentile URL to utilize. It is recommended to utilize sex-specific 99th percentile URLs, as women have lower levels of cTn compared to men.1,3 Use of an overall 99th percentile (which falls below the male-specific 99th percentile, and above the female-specific 99th percentile) in a male patient with a result near this threshold may lead to interpretation of the result as greater than the 99th percentile, when with use of a male-specific 99th percentile URL the result would be less than this threshold. The probability of this scenario is somewhat low, however, given the likelihood of cTn results that may be expected to occur close to the 99th percentile.
Biological-related cardiac troponin elevations
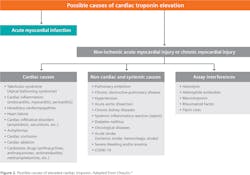
One of the first factors to consider when interpreting an elevated troponin result in the differential diagnosis of acute MI is a cause where the troponin is truly elevated, but due to disease other than acute MI, to assure the proper diagnosis and treatment are identified. Referring back to Figure 1, these mechanisms of myocardial cell injury may be acute non-ischemic (no cTn rise and/or fall) or may be chronic (cTn stable). These diseases can largely be grouped into two categories: 1) cardiac causes and 2) non-cardiac or systemic causes (Figure 2). Examples of cardiac diseases that may cause an elevated cTn include atrial fibrillation, myocarditis, and acute heart failure.1,4 Some cardiac disorders would have overlapping signs or symptoms with acute MI, such as shortness of breath, weakness, and even chest pain, meaning that the differential diagnosis must be carefully evaluated. Examples of non-cardiac or systemic disorders that may cause myocardial injury and elevated cTn include chronic kidney disease, pulmonary hypertension, stroke, and sepsis.1,4 For some cTnT assays, one source of elevation that has been published on consistently in the non-cardiac disorder group is skeletal muscle disease, which has been hypothesized to be due to re-expression of cTnT in the skeletal muscle.5,6 Another more recently discovered cause of increased cTn is COVID-19. A variety of cardiac or non-cardiac sources may cause a cTn increase in the clinical context of COVID-19, some of which may be non-ischemic but also ischemic, and the observed cTn concentration reflects a combination of what may be pre-existing cardiac disease and acute myocardial injury.7Assay-related cardiac troponin elevations
As with many laboratory assays, interferences may exert effects that assay design cannot mitigate or at least fully mitigate. Some of these interferences affect all assays, and some may affect only certain assays. Three common interferences that are regularly tested make up the HIL index, or hemolysis (hemoglobin), icterus (bilirubin) and lipemia (triglycerides/Intralipid; also called turbidity). As hemolysis increases, hs-cTnI and hs-cTnT results have been reported to increase (or decrease) for susceptible assays.8-10 Laboratories should seek out the assay Instructions for Use (IFU) from their manufacturer to understand the HIL interference criteria and limits for their assay.
Various types of endogenous antibodies may also affect cTn results, including heterophile antibodies, autoantibodies, and macrotroponin. Anti-troponin autoantibodies likely cause a falsely low result, and therefore are less concerning from the perspective of elevated cTn in the differential diagnosis of acute MI. Heterophile antibodies and macrotroponin, on the other hand, may cause falsely elevated (or falsely depressed) results. Heterophile antibodies are produced against poorly defined immunoglobulins, and have weak avidity to multi-specific antigens, generated from any number of environmental sources, certain infections, or some treatments. Prevalence estimates vary widely. When present in a patient sample, heterophile antibodies can cause falsely elevated results by cross-linking of the heterophile antibodies with the cTn antibodies used in the assay architecture. As has been reported since the late 1990s, this may cause a falsely elevated result, which has been reported in multiple case studies and reviewed.11,12
Macrotroponin interference can occur when autoantibodies bind cTn to make a complex. These large immunoglobulin-troponin complexes have reduced clearance and can affect assays differently and inconsistently. In other words, a particular assay may be affected by macrotroponin in one sample, but not be affected by macrotroponin in another sample.13 The results are often elevated above the 99th percentile, and sometimes very elevated, as demonstrated in a recent case study.14 Prevalence of macrotroponin has been suggested to be 5% or less,15 but our knowledge of prevalence, causes, and other aspects is currently limited.
Another potential cause of elevated cTn results is rheumatoid factor (RF), an interferent that may affect various analytes on immunoassay analyzers. Rheumatoid factor may be elevated in autoimmune diseases including rheumatoid arthritis and systemic lupus erythematosus, especially when the disease is active, such that the elevation is significant enough to cause an interference and false positive cTn. RF can cause significantly elevated results high above the 99th percentile URL.16
In addition to those interfering factors covered here, other factors that may cause falsely elevated cTn results should be considered when interpreting or investigating cTn elevations, including fibrin clots, sample type, time of day of blood draw (which has been reported to affect cTnT), and transportation of specimens.17-20
Conclusion
The proper interpretation of cTn elevations in the context of acute myocardial ischemia/infarction requires careful consideration of potential preanalytical and clinical causes of cTn elevation. In addition to many types of preanalytical factors, there may be analytical and clinical causes of troponin elevations, which may be from acute non-ischemic disease, or chronic disease that causes myocardial injury. The consideration for acute MI versus other cardiac or non-cardiac and systemic diseases, and communication with the laboratory if an analytical-related influence is suspected, will help ensure the patient receives the most accurate diagnosis and treatment plan.
References
1. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72(18):2231-2264. doi:10.1016/j.jacc.2018.08.1038.
2. Sandoval Y, Apple FS, Mahler SA, et al. High-sensitivity cardiac troponin and the 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guidelines for the evaluation and diagnosis of acute chest pain. Circulation. 2022;146(7):569-581. doi:10.1161/circulationaha.122.059678.
3. Apple FS, Sandoval Y, Jaffe AS, Ordonez-Llanos J. Cardiac troponin assays: Guide to understanding analytical characteristics and their impact on clinical care. Clin Chem. 2017;63(1):73-81. doi:10.1373/clinchem.2016.255109.
4. Chaulin AM. False-positive causes in serum cardiac troponin levels. J Clin Med Res. 2022;14(2):80-87. doi:10.14740/jocmr4664.
5. du Fay de Lavallaz J, Prepoudis A, Wendebourg MJ, et al. Skeletal muscle disorders: A noncardiac source of cardiac troponin T. Circulation. 2022;145(24):1764-1779. doi:10.1161/circulationaha.121.058489.
6. Jaffe AS, Vasile VC, Milone M, Saenger AK, Olson KN, Apple FS. Diseased skeletal muscle. J Am Coll Cardiol. 2011;58(17):1819-1824. doi:10.1016/j.jacc.2011.08.026.
7. Mueller C, Giannitsis E, Jaffe AS, et al. Cardiovascular biomarkers in patients with COVID-19. Eur Heart J Acute Cardiovasc Care. 2021;10:310-319. doi:10.1093/ehjacc/zuab009.
8. Harley K, Bissonnette S, Inzitari R, et al. Independent and combined effects of biotin and hemolysis on high sensitivity cardiac troponin assays. Clin Chem Lab Med. 2021;59:1431–1443. doi:10.1515/cclm-2021-0124.
9. Kavsak PA, Edge T, Roy C, et al. Analytical assessment of ortho clinical diagnostics high sensitivity cardiac troponin I assay. Clin Chem Lab Med. 2020;59:749–755. doi:10.1515/cclm-2020-1115.
10. Wei J, Wu YN, Ling Y, Chen XT, Zhu Q, Xu J. False decrease of high-sensitivity cardiac troponin T assay in pneumatic tube system samples. Clin Chim Acta. 2019;495:507–511. doi:10.1016/j.cca.2019.05.027.
11. Santos LG, Carvalho RR, Sá FM, et al. Circulating Heterophile Antibodies Causing Cardiac Troponin Elevation. An Unusual Differential Diagnosis of Myocardial Disease. JACC Case Reps. 2020;2:456-460. doi:10.1016/j.jaccas.2020.01.011.
12. Lippi G, Aloe R, Meschi T, Borghi L, Cervellin G. Interference from heterophilic antibodies in troponin testing. Case report and systematic review of the literature. Clin Chim Acta. 2013;426:79–84. doi:10.1016/j.cca.2013.09.004.
13. Kavsak PA, Roy C, Malinowski P, et al. Macrocomplexes and discordant high-sensitivity cardiac troponin concentrations. Ann Clin Biochem. 2018;55:500-504. doi:10.1177/0004563217734883.
14. Ghossein J, Ghossein J, Booth RA, Kavsak P, Chamoun C. Presence of Macrotroponin for Over 2 Years in a Young Woman. CJC Open. 2022;4:1012-1014. doi:10.1016/j.cjco.2022.07.016.
15. Warner JV and Marshall GA. High incidence of macrotroponin I with a high-sensitivity troponin I assay. Clin Chem Lab Med. 2016;54:1821-1829. doi:10.1515/cclm-2015-1276.
16. Saunders A, Tsui AKY, Alhulaimi N. Persistent Troponin Elevation in the Setting of an Elevated Rheumatoid Factor: When It Pays to Double Check. CJC Open. 2021;3:981-983. doi:10.1016/j.cjco.2021.02.014.
17. Kazmierczak SC, Sekhon H, Richards C. False-positive troponin I measured with the Abbott AxSYM attributed to fibrin interference. Int J Cardiol. 2005;101:27-31. doi:10.1016/j.ijcard.2004.03.008.
18. Simons J, Beach L, Clark L, Kavsak PA. Matrix and bilirubin interference for high-sensitivity cardiac troponin I. Clin Chim Acta. 2015;442:49-51. doi:10.1016/j.cca.2015.01.002.
19. Klinkenberg LJ, van Dijk JW, Tan FE, van Loon LJ, van Dieijen-Visser MP, Meex SJ. Circulating cardiac troponin T exhibits a diurnal rhythm. J Am Coll Cardiol. 2014;63:1788–95. doi:10.1016/j.jacc.2014.01.040.
20. Paul HA, Chi Q, Gifford JL, Seiden-Long I. Not T too! False elevations in high-sensitivity cardiac troponin T (hs-cTnT) following specimen transport. Clin Biochem. 2023;115:86-91. doi:10.1016/j.clinbiochem.2022.08.008.
About the Author

Kalen Nissen, PhD, DABCC, FAACC
serves as a Senior Director of Medical Sciences and Medical Officer for Diagnostics at Siemens Healthineers. Before joining Siemens Healthineers, she served as the Clinical Laboratory Director at a large healthcare system in the Minneapolis/St. Paul metropolitan area.