Current and future state of early cancer detection biomarkers
Cancer biomarkers are important in early cancer detection when cure rates are highest. For the past several decades, we have made limited progress towards biomarker development for early cancer diagnoses. We continue to rely on older biomarkers to screen for cancers including cervical, prostate and colon cancers. This article aims to examine some current cancer screening tests, detail barriers to progress in cancer biomarker screening, and outline what’s next for this important field of study.
Currently, the Papanicolaou test, also known as “the Pap,” exists as a pillar of women’s health and an important cancer detection tool. The Pap test was developed in the 1940s by Georgios Papanikolaou, MD, and it involves examination of exfoliating cells from the transformation zone of the cervix for detection of cancerous or precancerous lesions. The Pap has proven to be extremely effective at cervical cancer detection and has been critical to the dramatic decrease in cervical cancer incidence and mortality in the United States. The addition of human papillomavirus (HPV) with the Pap (co-testing) provides enhanced sensitivity for cervical cancer detection.1
For men, the prostate specific antigen (PSA) test was created with hopes it would have a similar impact on reducing prostate cancer. Indeed, the PSA test can detect prostate cancer approximately years earlier than a digital rectal exam and years before symptoms of the disease are recognized. The prostate cancer mortality rate in the US declined more than 40% since the early 1990s, when PSA screening became widespread.2 In recent years, concerns were raised about whether prostate cancer mortality had truly declined, and if the risks of diagnosis and treatment were substantial, relative to their benefits.
These tests are examples of older screening tests to detect cancer. Fortunately, there has been some progress with much of the most impactful recent advances supported by the National Cancer Institute (NCI). For example, a variety of projects in progress are currently evaluating liquid-based tests that could identify a variety of cancers early based on DNA fragments.3 One example, UroSEEK, is a urine-based test that detected the most common alterations in 11 genes linked to bladder and upper tract urothelial cancers. In a study, UroSEEK identified 83% of those who developed bladder cancer.4 Another project, PapSEEK, is similar, and aims to look at available DNA from specimens collected for Pap tests. In a study, the test was able to detect some endometrial and ovarian cancers at early, more treatable stages.5 Finally, CancerSEEK looks at circulating DNA and protein biomarkers. In a large trial of women with no history of cancer that combined the blood test with whole-body PET imaging, 65% of cancers that were detected were at an early stage.6 Given this information and the above projects, why has there not been more progress made in cancer biomarker screening?7
What are the primary issues?
Primary issues to overcome include cost and biomarker performance, i.e., false positives and false negatives. False positive screening test results push patients, in the absence of having the screened condition, to obtain follow-up or confirmatory testing. Follow-up tests can have substantial costs and may cause harm. False negative screening results leave patients with the screened condition unidentified, and the disease can progress. In addition, cost is a consideration, including the cost of the biomarker-based testing and associated costs including financial, risks of harm, time, and anxiety associated with a making the definitive diagnosis with follow-up diagnostics in both true (and any false) positives.
Cancer biomarkers must be carefully selected. For instance, CA-125 testing can help physicians in follow-up management of patients with ovarian carcinoma. Because a biomarker screening test for ovarian cancer does not exist, some providers may also use CA-125 to help screen patients. Yet, a study of 78,216 women ages 55 to 74 years of age who were randomly selected to receive either an annual CA -125 test and pelvic ultrasound screening or the usual medical care showed that CA-125 testing and ultrasound screening failed to reduce ovarian cancer deaths.8 The study also found that false-positive tests led to additional testing and procedures that sometimes resulted in serious complications.
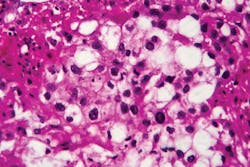
Biomarkers for bladder cancer screening have not proven to be successful and are not recommended by national guidelines, yet in surveillance for recurrence they have been shown to be useful.9 Cancer biomarkers can help decrease the need for an invasive procedure such as intravesical therapy (injection for early stage bladder cancer) and detect bladder cancer recurrence. The use of a screening test using fluorescence in situ hybridization (FISH) in urine samples in conjunction with cystoscopy has been shown to help in bladder cancer diagnosis in patients with hematuria who are suspected of having bladder cancer. The test may also detect cancer recurrence when a cystoscopy and urine cytology are equivocal. In a prospective study the test was beneficial in patients who had an atypical cytology and an equivocal or negative urine cytology.10 The combination of the procedure and the testing can help in ambiguous situations to further identify patients who truly have a recurrence from those who remain in remission.11
What’s next in Cancer Biomarker Development?
The National Cancer Institute (NCI) is spearheading several key initiatives to address the slow progress in early cancer biomarker development.12 This strategic approach will spur new research and evaluation of new diagnostics and therapeutics.
NCI’s Early Detection Research Network (EDRN), a collaborative consortium of academic and private-sector investigators, has focused on the systematic discovery, development, and validation of biomarkers and imaging methods to detect early-stage cancers and to assess risk for developing cancer. The goal of EDRN is to develop biomarkers that can distinguish aggressive early-stage cancers from slow-growing cancers that would never cause symptoms to reduce overtreatment.
Cancer researchers are turning to proteomics (the study of protein structure, function, and patterns of expression) and proteogenomics (the integration of proteomics with genomics and gene expression analysis, or transcriptomics, which involves the study of all RNA molecules in a cell.) with the hope of developing novel biomarkers that can be used to identify cancer in its early stages, to predict the effectiveness of treatment, and to predict the chance of cancer recurrence.
NCI’s Clinical Proteomic Tumor Analysis Consortium (CPTAC) is using a proteogenomic approach for tumor marker discovery for a growing number of cancers, including colorectal, breast, and ovarian cancers. By systematically identifying proteins (and associated biological processes) that originate from alterations in cancer genomes, CPTAC researchers have discovered new tumor subtypes, tumor microenvironment variations, and new potential proteins for targeted drug therapy. Recent innovations have suggested that these analyses could be done on a microscale using very small amounts of tumor tissue obtain from a biopsy.
NCI’s Molecular Applications for Therapy Choice (NCI-MATCH) and NCI-COG Pediatric MATCH clinical trials are using a precision medicine approach to assign patients to treatment by gene mutations in their tumors rather than by the type of cancer they have. By analyzing the response of patients to these targeted agents, and the underlying genomic alterations associated with these responses, researchers are identifying potentially new molecular targets for cancer therapy. Companion studies associated with these trials will also allow researchers to identify new biomarkers for determining response to therapies and for predicting treatment resistance.
The NCI Cancer Moonshot Biobank is working with patient participants at community hospitals around the country to encourage them to donate tissue and blood specimens over the course of their cancer treatment. The specimens are sent to researchers who use them to better understand cancer and potentially identify tumor markers.
Summary
The limited delivery of breakthroughs in early cancer biomarkers has been frustrating, but there is hope that new strategic investments by NCI, academics and diagnostic companies will be the stimulus for new diagnostic tools. The intersection of large datasets and artificial intelligence may provide clues to new approaches of evaluating risks (and targeting diagnostics to high-risk individuals), utilizing the best tests we have today while looking forward to new and better tests being developed. In the interim, we need to encourage people to be screened with cancer biomarkers that have been proven to be effective such as for cervical cancer, colorectal cancer, and, when indicated with appropriate consultation, prostate cancer.
Increased adherence to guidelines will have dramatic impacts in driving down cancer prevalence and mortality. Furthermore, the COVID-19 pandemic has left a gap of people who have skipped or delayed routine healthcare services, including cancer screening.13 We must be proactive in safely closing the gap in care with biomarker-based screening, in most cases, having the fewest barriers for large scale implementation. Although current testing has challenges and nuances as discussed, it offers the ability to screen large numbers of patients who may have delays in care, which, if not addressed, have the potential to increase cancer related morality.
References:
- Kaufman HW, Alagia DP, Chen Z, Onisko A, Austin RM. Contributions of liquid-based (Papanicolaou) cytology and human papillomavirus testing in cotesting for detection of cervical cancer and precancer in the United States, Am J Clin Pathol. 2020;154:510-516. doi: 10.1093/ajcp/aqaa074.
- Brawley OW. Trends in prostate cancer in the United States. J Natl Cancer Inst Monogr. 2012;2012(45):152-156. doi:10.1093/jncimonographs/lgs035.
- Bettegowda C, Sausen M, Leary RJ, et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 2014; 6(224):224ra24. doi: 10.1126/scitranslmed.3007094.
- Springer SU, Chen CH, Rodriguez Pena MDC, et al. Non-invasive detection of urothelial cancer through the analysis of driver gene mutations and aneuploidy. Elife. 2018;7:e32143 doi: 10.7554/eLife.32143.
- Wang Y, Li L, Douville C, et al. Evaluation of liquid from the Papanicolaou test and other liquid biopsies for the detection of endometrial and ovarian cancers. Sci Transl Med. 2018; 10(433):eaap8793. doi: 10.1126/scitranslmed.aap8793.
- Lennon AM, Buchanan AH, Kinde I, et al. Feasibility of blood testing combined with PET-CT to screen for cancer and guide intervention. Science. 2020; 369(6499):eabb9601. doi: 10.1126/science.abb9601.
- Duffy MJ. Clinical uses of tumor markers: a critical review. Crit Rev Clin Lab Sci. 2001:38(3):225-262, doi: 10.1080/20014091084218.
- Buys SS, Partridge E, Black A, et al. Effect of Screening on Ovarian Cancer Mortality: The Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Randomized Controlled Trial. JAMA. 2011;305(22):2295–2303. doi:10.1001/jama.2011.766.
- Rodriguez-Homs, M, Baack Kukreja, J. Bladder cancer biomarkers: Past and future directions. BJUI Compass. 2021; 2: 7– 8. doi.org/10.1002/bco2.61
- Bangma CH, Loeb S, Busstra M, et al. Outcomes of a bladder cancer screening program using home hematuria testing and molecular markers. Eur Urol. 2013;64(1):41-7. doi: 10.1016/j.eururo.2013.02.036.
- Schlomer BJ, Ho R, Sagalowsky A, et al. Prospective validation of the clinical usefulness of reflex FISH assay in patients with atypical cytology for the detection of urothelial carcinoma of the bladder. J Urol. 2010; 183(1):62-7. doi: 10.1016/j.juro.2009.08.157.
- Cancer Biomarkers | Division of Cancer Prevention, EDRN — Early Detection Research Network (nih.gov), CPTAC | Office of Cancer Clinical Proteomics Research, NCI-MATCH Precision Medicine Clinical Trial - National Cancer Institute, and Cancer Moonshot — National Cancer Institute Accessed October 15, 2021.
- Kaufman HW, Chen Z, Niles JK, Fesko YA. Changes in Newly Identified Cancer Among US Patients From Before COVID-19 Through the First Full Year of the Pandemic. JAMA Netw Open. 2021;4(8):e2125681. doi:10.1001/jamanetworkopen.2021.25681.
About the Author

Yuri A. Fesko, MD
a board-certified oncologist, is Executive Medical Director of Medical Affairs at Quest Diagnostics.

Harvey W. Kaufman, MD
a board-certified pathologist, is Senior Medical Director at Quest Diagnostics. A 29-year veteran of Quest Diagnostics, Kaufman was an original and still active member of the Laboratory Working Group of the National Institute of Diabetes and Digestive and Kidney Diseases, NIH (formerly the National Kidney Disease Education Program).