Review of laboratory diagnostic tests for invasive aspergillosis
LEARNING OBJECTIVES
1. Recall aspergillosis causative agents and describe its disease complications.
2. Discuss classification of diagnosis of Aspergillus disease based on EORT/MSG and the AspICU.
3. Describe all laboratory testing methods for the diagnosis of Aspergillus disease and their limitations.
4. Discuss the future recommendations for the proper diagnosis of Aspergillus disease.
Aspergillus species, which are common environmental fungi, are known to cause aspergillosis, an invasive infection commonly observed in people with a weakened immune system. The most common Aspergillus species causing human disease are A. fumigatus, A. flavus, A. terreus, and A. niger, which can cause a wide range of clinical syndromes, such as allergic bronchopulmonary aspergillosis, aspergilloma, chronic pulmonary aspergillosis, and invasive aspergillosis. Aspergillus is widespread in the environment and can colonize the airway, making diagnoses of invasive pulmonary aspergillosis difficult to differentiate from colonization. Aspergillosis is one of the most commonly missed diagnoses in ICU patients based on a systematic review of autopsy studies.1 Therefore, being suspicious of a possible aspergillosis infection and having the ability to diagnose it with the help of lab tests is critical.
Cases of invasive pulmonary aspergillosis that occur in critically ill patients with viral pneumonia have been reported recently.2 Influenza-associated pulmonary aspergillosis (IAPA) has been reported globally with a variety of influenza strains with mortality rates as high as 57 percent.2
Because laboratory diagnostics are critical in the early detection and management of invasive aspergillosis per guidelines, it is important for laboratory scientists to be familiar with the range of diagnostic tests used in clinical practice. Two commonly used case definitions for invasive aspergillosis – by the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Disease Mycoses Study Group (EORTC/MSG), as well as the AspICU collaboration – 3, 4 require mycological evidence for the diagnosis of invasive aspergillosis. In the EORTC/MSG definition, Aspergillus-positive culture, galactomannan antigen detected, or Aspergillus-positive Polymerase Chain Reaction (PCR), are acceptable mycological evidence when aspergillosis host factors and clinical features are also present.3 For the AspICU clinical algorithm, which was developed more for clinical trials than patient care, an Aspergillus-positive culture is an entry criteria for diagnosing aspergillosis in addition to clinical symptoms, abnormal radiographic features, and host factors.4
We will review specimen collection procedures first and then commonly used tests to detect invasive aspergillosis, such as conventional diagnostics, immunodiagnostic, molecular tests and novel laboratory approaches. Lastly, Aspergillus, species antifungal susceptibility testing will be briefly discussed as well.
Literature review
We conducted a review of published literature including conferences abstracts and full papers to identify studies that investigated aspergillosis diagnostic test performance. We searched PubMed and Google Scholar using keywords “aspergillosis,” “diagnostic tests,” “beta-D-glucan,” “galactomannan,” “lateral flow assay,” “culture,” “histopathology,” “microscopy,” “anti-fungal susceptibility tests,” “polymerase chain reaction,” “next generation sequencing,” and “volatile organic compounds.” The range of reported sensitivity, specificity, and reproducibility from reported articles and commercial assay reports were extracted and the Aspergillus diagnostic tests were classified into three main categories: conventional diagnostics, immunodiagnostics, and molecular diagnostics. We summarized the strengths and weaknesses for different tests in each category and discussed isolate identification and antifungal susceptibility testing.
Specimens for invasive aspergillosis diagnosis
A key step to diagnosing aspergillosis is to select the right sample specimen for laboratory testing, since a poor-quality specimen can result in inaccurate laboratory results. While cerebrospinal fluid (CSF) and urine have been used, serum and lower respiratory tract specimens (bronchoalveolar lavage, sputum, or tracheal aspirate) are commonly used for aspergillosis diagnosis.5 Since Aspergillus is commonly found in the environment, there is a possibility of contamination during the venipuncture. Thus, prior to collecting blood, it is important to use iodine tincture or chlorhexidine wipes to decontaminate the blood collection site.5 Based on the laboratory diagnostic system used, the recommended amount of blood should be collected. Blood can easily be transported at room temperature to the laboratory without concerns that ambient temperature transport will affect lab results.5 Since blood is a sterile sample, detection of Aspergillus would indicate an infection of invasive aspergillosis. Lower respiratory tract samples, however, are susceptible to contamination, since Aspergillus can colonize the airways or lungs, with reported frequencies of 36-91 percent, but not cause infection, especially in patients with chronic lung disease.6 Thus, the collection procedure for lower respiratory tract samples is important. It is recommended that sputum samples be collected in the morning right after brushing teeth.5 All bronchoalveolar lavage specimens should be collected via bronchoscopy, and all lower respiratory tract specimens should be collected using a sterile tube. Lower respiratory tract specimens can be transported to the laboratory within two hours at room temperature, but if one requires longer time for transportation, the specimen should be kept at 4°C.5 Since a lower respiratory tract specimen is not sterile, it is difficult to associate a positive test result with infection and a blood/serum sample might be needed.6
Conventional Diagnostics
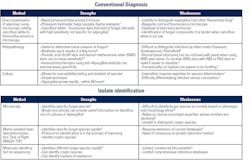
Conventional diagnostics rely on culture and microscopy for staining and visualization. Direct examination of the respiratory specimen under the microscope for Aspergillus is one such example of conventional diagnostics. Direct examination allows rapid turnaround times of 2–4 hours. Technique could be improved by staining the specimen with calcofluor white and 10 percent potassium hydroxide to provide better sensitivity, since calcofluor white is a fluorescent dye that binds to the fungal cell wall, and potassium hydroxide helps visualize the hyphae of the fungus by dissolving the walls of human epithelial cells.7 In addition to the cost for reagents and a fluorescence microscope, the main downside of direct examination is the difficulty to distinguish Aspergillus from other fungi with filamentous elements, which would require an experienced microscopist (Table 1).7
Culture
The most widely available conventional diagnostic for Aspergillus is fungal culture. Its wide availability stems mainly from a clinical aspect since a positive Aspergillus fungal culture is useful for diagnosing invasive aspergillosis. Fungal culture is a relatively simple technique, and most Aspergillus species grow rapidly in a fungal culture plate within 48 hours. A variety of solid and liquid fungal media can be used for growing Aspergillus, such as blood agar, chocolate agar, brain heart infusion broth, Czapeck agar, potato dextrose agar, cornmeal agar, and Sabouraud dextrose agar.7 Additionally, antibiotics, such as chloramphenicol and gentamicin, are added to the fungal culture to prevent bacterial growth.7 Besides antibiotics, protein synthesis inhibitors such as cycloheximide are occasionally added to inhibit environmental mold growth; although, this can also inhibit Aspergillus.7 Fungal culture also allows for antifungal susceptibility testing. The drawback of fungal culture is that it is difficult to differentiate clinical colonization from infection and often requires an expert to be able to determine the species of the fungi.7 Books and online articles that provide useful information on identification of common Aspergillus species are available (Table 1).
Histopathology
Histopathology, another type of conventional diagnostic, can be useful to determine whether the fungus is invasive within tissue and provides relatively quick results within 2-3 days. Most pathology and laboratory professionals use haemotoxylin and eosin (H&E) staining; however, studies have reported increased sensitivity when using Periodic acid-Schiff (PAS) stain and Grocott’s (Gomori) methenamine silver stain (GMS).8 For suspected aspergillosis, experts advise using H&E counterstaining and either GMS or PAS staining simultaneously to avoid delays in reporting results.8 Despite histopathology’s ability to determine invasion, microscopy cannot easily distinguish Aspergillus from other molds, such as Fusarium, Scedosporium, and Penicillium.8 However, using immunohistochemistry with anti-Aspergillus antibody can reduce the difficulty of distinguishing Aspergillus from Candida, Fusarium, Mucorales, Scedosporium, Paeciliomyces, and dematiaceous fungi (Table 1).
Immunodiagnostics
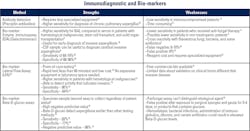
Immunodiagnostic assays are used to detect pathogen-specific antigens or antibodies produced against foreign antigens. These tests are based on the antibody-antigen complex formation. Commonly used immunodiagnostics are galactomannan and beta-D-glucan tests, which are antigen tests (Table 2).
Galactomannan
Galactomannan is a cell wall component of Aspergillus. Immunodiagnostics assays that detect galactomannan antigen have been useful for the rapid, early detection of invasive aspergillosis. Serum and bronchoalveolar lavage fluid have been used as sample specimens.9 The sensitivity of antigen detection in bronchoalveolar lavage fluid is higher when compared with serum in patients at high risk of developing aspergillosis, such as patients with hematological malignancies. Cerebrospinal fluid (CSF) specimens have been reported as useful specimens for the diagnosis of cerebral invasive aspergillosis, but the use of these types of samples lack validation studies.9
Previous studies of galactomannan enzyme immunoassay (EIA) have reported good sensitivity and specificity. In a meta-analysis that analyzed twenty-seven studies of patients with immunosuppression (hematological malignancy or bone marrow or solid organ transplant), Pfeiffer and colleagues reported the pooled sensitivity and specificity of the galactamannan EIA for proven invasive aspergillosis cases as 71 percent and 89 percent.10 The pooled sensitivity was 61 percent and pooled specificity was 93 percent when probable invasive aspergillosis cases were included.10
A few commercial kits are available for galactomannan EIA, but only one is well validated and widely available. Despite its ease of use, galactomannan EIA might not be used in routine clinical care for several reasons. Clinically, galactomannan EIA has lower sensitivity in non-neutropenic patients and patients who have already received antifungal medications.11 False positive results can also occur due to recent use of antibiotics – such as amoxicillin/clavulanic acid, piperacillin-tazobactam, and beta-lactam antibiotics – or other bacterial or fungal infections, such as with Penicillium, Alternaria, Paecilomyces, and Histoplama.
In addition to the varied clinical performance, another drawback is the reagent cost and the specialized equipment necessary to perform the test (Table 2).12
Lastly, Aspergillus lateral flow assays (LFAs) have been developed as a rapid, point-of-care test to detect an Aspergillus galactomannan antigen or an Aspergillus specific extracellular glycoprotein antigen. A primary benefit of LFAs is their low cost, because LFAs do not require expensive equipment or laboratory space. Thus, they can be utilized in low-resource settings to diagnose invasive aspergillosis. The specimen sample can be serum or bronchoalveolar lavage fluid. The test sensitivity and specificity are high, 90 percent and 84 percent respectively.13 Higher sensitivity has been reported in patients with hematological malignancies. The assay that uses a monoclonal antibody, which binds to an Aspergillus specific antigen, does not cross-react with other antibiotic drugs.13 Additionally, LFAs that detect antigen in serum specimens suggest that the infection is invasive, an important aspect for determining the clinical significance of infection.13 However, a limited number of commercial LFA kits are available. Data on LFAs in clinical use is limited; thus, more research is needed (Table 2).
Beta-D-glucan
Another type of rapid immunodiagnostics is the beta-D-glucan assay, which uses serum as the specimen sample. Beta-D-glucan is another fungal cell wall component; however, the fungal antigen is not specific to Aspergillus. There is a beta-D-glucan antigen detection assay kit available for clinical laboratories that is commonly used and widely available. Using the assay involves creating a standard curve of beta-D-glucan levels, incubation of the sample and reading the assay plate. Most have a sensitivity of 93 percent and specificity of 77 percent.14 In comparison with the galactomannan antigen EIA, the beta-D-glucan assay has a higher sensitivity and negative predictive value but a lower specificity.14 False positives can also result from exposure to external glucan antigens found on surgical sponges and gauze, immunoglobulins, albumin, beta-lactam antibiotics, hemodialysis, tubes for sample collection, developing bacterial infections, and other causes. Besides the low specificity, another limitation of the beta-D-glucan assay is the cost of performing the test, given the concern for false-positives and false-negatives (Table 2).
Immune precipitation
In immune precipitation, the antibody and antigen diffuse towards each other in the gel and create a band called a precipitin band. That process does require less specialized equipment to detect aspergillosis as compared to microscopy.12 However, immune precipitation is time consuming and may take up to two to three days to obtain results.12 As more immunodiagnostic assays became readily available, galactomannan and beta-D-glucan tests became more favored over the precipitin test. Immunodiagnostic assays that rely on antibody (Ab) testing are good for immunocompetent patients. However, in immunocompromised patients, those antibody assays are less sensitive due to inadequate antibody production in response to the infection. In these situations, an antigen detection assay has better analytical performance.
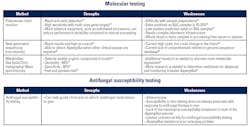
Molecular diagnostics
The most commonly used molecular diagnostic is polymerase chain reaction, which provides rapid detection of Aspergillus species using bronchoalveolar fluid and serum as specimen samples, with bronchoalveolar fluid having a higher risk of false positive results, because it is not sterile. The drawback of PCR tests for Aspergillus is the lack of standardized protocols across different laboratories, the difficulty with preparing samples, and the false positive frequency when using non-sterile samples.15 Studies have reported higher sensitivity when multi-copy gene targets are used and when whole blood instead of serum is used.15 However, whole blood is more difficult to process for PCR, and data is limited on its higher sensitivity.15 Typically, PCR target genes include 18S rRNA, 28s rRNA, mtDNA, and internal transcribed spacer (ITS).15, 16 Additionally, more advanced equipment, such as automated processors, can reduce performance variability compared to manual processing, but this advanced equipment costs more and requires more complex laboratory infrastructure than other types of diagnostics (Table 3). In a meta-analysis of 16 studies that included adult and children with hematological malignancy or hemopoietic stem-cell transplant, Mengoli and colleagues showed that the pooled sensitivity and specificity for one PCR-positive test was 88 percent and 75 percent, which was useful enough to exclude invasive aspergillosis.16 However, they concluded that two PCR-positive tests were necessary to confirm an invasive aspergillosis diagnosis based on the pooled sensitivity and specificity for two PCR-positive tests of 75 percent and 87 percent respectively.16 As of 2016, the Infectious Disease Society of America does not recommend Aspergillus PCR for clinical use, because experts do not agree on the utility of PCR in clinical diagnosis. Few commercial assays are validated, and there is a lack of standardization in Aspergillus PCR methods.17
A less commonly used specimen for molecular diagnostics is formalin fixed paraffin embedded (FFPE) tissue. Molecular testing of FFPE samples is possible using nine polymorphic short tandem repeat loci as well as detection of genes described previously in the PCR testing section above.18 DNA is extracted from FFPE lung biopsies by lysing cells and purified through affinity chromatography.18 After DNA extraction, genotyping was done using PCR. Azole susceptibility could be tested by identifying CYP51A mutations such as TR34, L98H, Y121F, and T289A.19 Studies have reported that this method is capable of detecting Aspergillus in FFPE samples 41-94 percent of the time (Table 3).18
Next generation sequencing
An infrequently used molecular test due to its high costs is next generation sequencing, which can provide rapid and highly accurate results for diagnosing invasive aspergillosis.20 Some studies have reported that next generation sequencing is able to detect Aspergillus when other assays cannot.20 Differentiating invasive aspergillosis from colonization is clinically important, as missing the diagnoses can result in delayed treatment and consequently death.20 In contrast, Aspergillus colonization in the airway is relatively common, and overtreatment may be deleterious to the patient.20 The main weakness of next generation sequencing, however, is the lack of a comprehensive reference genome sequence database (Table 3).20
Recently, detection of Aspergillus metabolites has been developed using gas liquid chromatography/mass spectroscopy. The premise is that gas liquid chromatography/mass spectroscopy can detect volatile organic compounds, which are produced by Aspergillus, in the breath.21 It is a fast and painless test with reported sensitivities of 94 percent and specificity of 93 percent.21 However, additional research is needed to uncover new Aspergillus metabolite signatures and to determine its effectiveness for diagnosing invasive aspergillosis.21
Isolate identification
In addition to detecting Aspergillus, it is important to identify the species of the fungus. There are a few methods developed for isolate identification, such as microscopy, matrix-assisted laser desorption/ionization-time of flight (MALDI-TOF), and PCR with sequencing. Although microscopy can identify the genus and species of fungi, it is difficult to reliably characterize the species based on morphology alone, and it relies heavily on a mycologist’s expertise.21 Another downside of microscopy is that it is unable to distinguish cryptic species of Aspergillus, which are defined as species that are morphologically indistinguishable. MALDI-TOF and genetic sequencing can overcome that challenge and identify cryptic species. However, both lack a comprehensive reference database for identification.21 Internal transcribed spacer sequencing has limited commercial kits available for isolate identification; whereas, MALDI-TOF has an established extraction protocol for commercial equipment (Table 1).
Antifungal susceptibility testing (AFST)
An important aspect of Aspergillus testing is AFST due to its clinical relevance, especially since resistance to commonly used antifungal medications in Aspergillus fumigatus has been increasing.19 There are two types of resistance: intrinsic resistance, which is resistance that is natural and innate part of the fungus that emerges when the species emerges, and acquired resistance, which is resistance after exposure to antifungal medications.19 Resistant strains of Aspergillus mean certain antifungals are not effective and use of these antifungals may result in unfavorable clinical outcomes. Azole-resistant Aspergillus, particularly Aspergillus fumigatus, have been reported with increasing frequencies ranging from 1-15 percent, depending on the country due to a mutation of the CYP51A, which is an azole target.19 However, there are methods for detecting azole-resistant Aspergillus by looking for markers, such as TR34/L98H and TR46/Y121F/T289A.19 Additionally, other mutations for the CYP51A gene, such as G54R/W/E, M220I/K/V, P216L, F332K, and G448S have been reported.22
AFST is a slow and technically demanding process that requires growing the fungal specimen in culture with discs of varying concentration of the antifungal substance. The most common antifungal medications tested for susceptibility are amphotericin B, anidulafungin, caspofungin, micafungin, isavuconazole, posaconazole, itraconazole and voriconazole. Broth dilution is another method used to measure the minimum inhibitory concentration of antifungal drugs and determine susceptibility. The broth dilution AFST method has been standardized by the Clinical and Laboratory Standards Institute (CLSI), which has a single breakpoint and epidemiologic cutoff values, and the European Committee on Antimicrobial Susceptibility Testing (EUCAST), which has breakpoints and epidemiologic cutoff values. Commercial kits are also available and compare how well Aspergillus grows on the commercial growth agar with no antifungal agent, itraconazole, voriconazole, and posaconazole. However, susceptibility in vitro does not always predict how Aspergillus will respond to antifungal treatment clinically (Table 3).
Recently published studies have been utilizing MALDI-TOF MS to type and test for antifungal susceptibility for Aspergilli.23 A few studies have looked at using MALDI-TOF MS for A. fumigatus and A. lentulus to provide quicker results for antifungal susceptibility.23 The assay developed by Sanguinetti and Posteraro involves incubating the fungi with serial antifungal concentrations for 15 hours before analysis with MALDI-TOF, which allowed them to measure the minimal profile change correlation index, an alternative to the minimum inhibitory concentration.23 Future directions in using MALDI-TOF MS for AFST involves reducing the time needed to obtain results and testing the accuracy of the method.
Diagnosis difficult despite range of testing options
The wide variety of laboratory diagnostics tests available to detect Aspergillus species provides information about the Aspergillus infection, such as genus and species, invasion into other tissues, and susceptibility to antifungals. Conventional diagnostics allow us to visualize and diagnose aspergillosis through microscopes, fungal culture, and staining techniques, but takes valuable time to provide results back to the clinician, which would delay treatment. On the other hand, immunodiagnostics – such as galactomannan and beta-D-glucan detection, and novel lateral flow assays – provide rapid results through the detection of biomarkers. Newer developments in molecular diagnostics – such as PCR, MALDI-TOF MS and volatile organic compound detection diagnostics – could provide rapid, accurate tests but will require further research and expansion of current reference databases for Aspergillus.
Studies have found that a combination of diagnostic assays – such as PCR with culture, PCR with beta-D-glucan, PCR with galactomannan, galactomannan with beta-D-glucan – have provided better diagnostic accuracy.24, 25 For example, when the lateral flow assay that detects an Aspergillus-specific antigen is combined with PCR, sensitivity of greater than 94 percent and specificity of greater than 86 percent are reported.24 Galactomannan and PCR tests are reported to have high rates of agreement between the two assays (greater than 94 percent) in patients with hematologic malignancies, solid tumor malignancies, stem cell transplants, and primary or hereditary immunodeficiencies.25 Therefore, experts suggest a combination of galactomannan and PCR for diagnosis of invasive aspergillosis in patients with hematologic malignancies, solid organ transplant, and stem cell transplants. However, a limitation is that the combination of immunodiagnostics and molecular testing do not confirm a proven invasive aspergillosis case, since that requires a tissue biopsy and histological techniques. Perhaps immunodiagnostic and molecular tests could be incorporated in future guidelines for confirming an aspergillosis diagnosis.
Despite the diagnostic tools at our disposal to detect aspergillosis, the clinical diagnosis of aspergillosis is still difficult and often relies on clinical guidelines, such as the EORTC/MSG and AspICU diagnostic criteria.3, 4 The EORTC/MSG guidelines were created for the classical immunocompromised host for aspergillosis with classifications as proven, probable, and possible with probable based on three categories: (1) host risk factors such as neutropenia, hematologic malignancy, or allogenic stem cell transplant, (2) clinical features such as halo, crescent, or cavitary sign on chest CT, and (3) mycological evidence from fungal culture, galactomannan test, or Aspergillus PCR.3
Classical cases of invasive aspergillosis are common in an immunocompromised host, since aspergillosis is an opportunistic fungus. However, more recent studies have reported aspergillosis in immunocompetent patients, some of whom might be critically ill with influenza.2 These patients would typically not meet the classical EORTC/MSG criteria and do not typically display angioinvasion, which is a common level of invasion in an immunocompromised host.
The AspICU diagnostic criteria was developed for patients in the ICU without classic risk factors for aspergillosis. The criteria are (1) a positive Aspergillus culture, (2) clinical signs and symptoms such as dyspnea, hemoptysis, or pleuritic chest pain, (3) abnormal chest radiographic imaging, and (4) host risk factors that include high glucocorticoid treatment (>20mg prednisone equivalent).4
The need for increased awareness and education surrounding the diagnosis of invasive aspergillosis is critical. Finally, laboratory testing, especially for the detection of biomarkers and DNA, plays an important role in the control of Aspergillus outbreaks in hospitals, which have been seen due to contaminated water, ventilation systems, medicines and medical devices.
Our review had several limitations. One is that this was not a systematic literature review, and we did not attempt to include every reported diagnostic, but only those used in common clinical microbiology practice. Second, we did not perform a pooled analysis of the sensitivity, specificity, and reproducibility for the different diagnostic tests, and instead reported a range of values that were available.
Future efforts on aspergillosis diagnostics are focused on developing rapid, highly sensitive, and highly specific tests, such as lateral flow assays and volatile organic compound detection tests. Additionally, research is moving towards finding the best clinical algorithm for the diagnosis of aspergillosis, given the complexity of the different disease states.
Acknowledgements
The authors also would like to acknowledge the contributions from:
Karlyn Beer, MS, PhD, is an Epidemiologist at the Mycotic Diseases Branch, Division of Foodborne, Waterborne and Environmental Diseases for the Centers for Disease Control and Prevention. Tom Chiller, MD, MPHTM, is the chief of the Mycotic Diseases Branch in the Division of Foodborne, Waterborne and Environmental Diseases at the Centers for Disease Control and Prevention.
In addition, Diego H. Caceres acknowledges Oak Ridge Institute for Science and Education.
References
- Winters B, Custer J, Galvagno SM, et al. Diagnostic errors in the intensive care unit: a systematic review of autopsy studies. Bmj Quality & Safety. 2012;21(11):894-902. doi:10.1136/bmjqs-2012-000803.
- Shah MM, Hsiao EI, Kirsch CM, Gohil A, Narasimhan S, Stevens DA. Invasive pulmonary aspergillosis and influenza co-infection in immunocompetent hosts: case reports and review of the literature. Diagn Microbiol Infect Dis. 2018;91(2):147-152. doi:10.1016/j.diagmicrobio.2018.01.014.
- Donnelly JP, Chen SC, Kauffman CA, et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease From the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clinical Infectious Diseases. 2019;71(6):1367-1376. doi:10.1093/cid/ciz1008.
- Blot SI, Taccone FS, Van den Abeele AM, et al. A clinical algorithm to diagnose invasive pulmonary aspergillosis in critically ill patients. Am J Respir Crit Care Med. 2012;186(1):56-64. doi:10.1164/rccm.201111-1978OC.
- Karin L. Mcgowan. Specimen Collection, Transport, and Processing: Mycology. vol 2. Manual of Clinical Microbiology. American Society for Microbiology; 2015.
- Tashiro T, Izumikawa K, Tashiro M, et al. Diagnostic significance of Aspergillus species isolated from respiratory samples in an adult pneumology ward. Medical Mycology. 2011;49(6):581-587. doi:10.3109/13693786.2010.548084.
- Hope WW, Walsh TJ, Denning DW. Laboratory diagnosis of invasive aspergillosis. Lancet Infect Dis. 2005;5(10):609-22. doi:10.1016/S1473-3099(05)70238-3.
- Denning DW, Kibbler CC, Barnes RA, British Society for Medical M. British Society for Medical Mycology proposed standards of care for patients with invasive fungal infections. Lancet Infect Dis. 2003;3(4):230-40. doi:10.1016/s1473-3099(03)00580-2.
- Barton RC. Laboratory diagnosis of invasive aspergillosis: from diagnosis to prediction of outcome. Scientifica (Cairo). 2013;2013:459405. doi:10.1155/2013/459405.
- Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis. May 15 2006;42(10):1417-27. doi:10.1086/503427
- Marr KA, Laverdiere M, Gugel A, Leisenring W. Antifungal therapy decreases sensitivity of the Aspergillus galactomannan enzyme immunoassay. Clin Infect Dis. 2005;40(12):1762-9. doi:10.1086/429921.
- Page ID, Richardson M, Denning DW. Antibody testing in aspergillosis--quo vadis? Med Mycol. 2015;53(5):417-39. doi:10.1093/mmy/myv020.
- Heldt S, Hoenigl M. Lateral Flow Assays for the Diagnosis of Invasive Aspergillosis: Current Status. Curr Fungal Infect Rep. 2017;11(2):45-51. doi:10.1007/s12281-017-0275-8.
- Pickering JW, Sant HW, Bowles CA, Roberts WL, Woods GL. Evaluation of a (1->3)-beta-D-glucan assay for diagnosis of invasive fungal infections. J Clin Microbiol. 2005;43(12):5957-62. doi:10.1128/JCM.43.12.5957-5962.2005.
- Chen SC, Halliday CL, Meyer W. A review of nucleic acid-based diagnostic tests for systemic mycoses with an emphasis on polymerase chain reaction-based assays. Med Mycol. 2002;40(4):333-57. doi:10.1080/mmy.40.4.333.357.
- Mengoli C, Cruciani M, Barnes RA, Loeffler J, Donnelly JP. Use of PCR for diagnosis of invasive aspergillosis: systematic review and meta-analysis. Lancet Infect Dis. 2009;9(2):89-96. doi:10.1016/S1473-3099(09)70019-2.
- Patterson TF, Thompson GR, Denning DW, et al. Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America. Clinical Infectious Diseases. 2016;63(4):E1-E60. doi:10.1093/cid/ciw326.
- Springer J, McCormick Smith I, Hartmann S, et al. Identification of Aspergillus and Mucorales in formalin-fixed, paraffin-embedded tissue samples: Comparison of specific and broad-range fungal qPCR assays. Med Mycol. 2019;57(3):308-313. doi:10.1093/mmy/myy041.
- Mayr A, Lass-Florl C. Epidemiology and antifungal resistance in invasive Aspergillosis according to primary disease: review of the literature. Eur J Med Res. 2011;16(4):153-7. doi:10.1186/2047-783x-16-4-153.
- Kidd SE, Chen SC, Meyer W, Halliday CL. A New Age in Molecular Diagnostics for Invasive Fungal Disease: Are We Ready? Front Microbiol. 2019;10:2903. doi:10.3389/fmicb.2019.02903
- Terrero-Salcedo D, Powers-Fletcher MV. Updates in Laboratory Diagnostics for Invasive Fungal Infections. J Clin Microbiol. 2020;58(6). doi:10.1128/JCM.01487-19.
- Rivero-Menendez O, Alastruey-Izquierdo A, Mellado E, Cuenca-Estrella M. Triazole Resistance in Aspergillus spp.: A Worldwide Problem? J Fungi (Basel). 2016;2(3). doi:10.3390/jof2030021.
- Sanguinetti M, Posteraro B. MALDI-TOF mass spectrometry: any use for Aspergilli? Mycopathologia. 2014;178(5-6):417-26. doi:10.1007/s11046-014-9757-1.
- Boch T, Spiess B, Cornely OA, et al. Diagnosis of invasive fungal infections in haematological patients by combined use of galactomannan, 1,3-beta-D-glucan, Aspergillus PCR, multifungal DNA-microarray, and Aspergillus azole resistance PCRs in blood and bronchoalveolar lavage samples: results of a prospective multicentre study. Clinical Microbiology and Infection. 2016;22(10):862-868. doi:10.1016/j.cmi.2016.06.021.
- Vrioni G, Theodoridou K, Tsiamis C, et al. Use of Galactomannan Antigen and Aspergillus DNA Real-time Polymerase Chain Reaction as Routine Methods for Invasive Aspergillosis in Immunosuppressed Children in Greece. Clinical Therapeutics. 2018;40(6):918-924. doi:10.1016/j.clinthera.2018.05.002.
About the Author

John Z. Deng, BS
is with David Geffen School of Medicine at University of California Los Angeles (UCLA).

Diego H. Caceres, BSc, MSc
is an Epidemiologist at the Mycotic Diseases Branch, Division of Foodborne, Waterborne and Environmental Diseases at the Centers for Disease Control and Prevention.