Longitudinal performance of mRNA-based HPV testing as compared to DNA-based testing
Cervical cancer mortality has declined substantially since the 1971 introduction of cervical cancer screening by cytology (Pap smear). Moreover, the recognition that long-term (persistent) infection with any one of 13 high-risk human papillomaviruses (HPVs) may cause precancerous and malignant cervical lesions has led to the introduction of HPV testing as a co-test to cytology.4 HPV testing offers improved sensitivity and results in earlier detection of abnormalities that are likely to progress to cancer compared to cytology alone.3,7,8 A lower risk of cancer or high-grade neoplasia being detected at a second screening has prompted suggestions that the interval between screenings can be safely extended beyond three years.7 This is beneficial because more than 80 percent of HPV infections clear spontaneously within two to three years of detection, making it advantageous to maintain screening intervals of at least three years in order to avoid mistaking transient for persistent infections and overtreating the women tested.
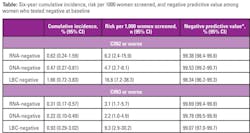
*NPV was estimated excluding the risk among those attending the second round of screening
DNA-based HPV testing: sensitive but not sufficiently specific
There are numerous HPV tests available, and combined Pap and HPV testing (co-testing) is now widely accepted as the best means of realizing additional reductions in cervical cancer through the recognition and prompt (early) treatment of high-risk HPV-positive lesions before they progress to cancer.1,9 Combined testing does not increase the burden for patients, as the two tests can be performed using a single swab. However, questions remain about the preferred method for HPV testing in screening protocols.
At present, there are nearly 200 tests for HPV, which include a number of nucleic-acid based tests. Among these, DNA-based tests have proven higher sensitivity; however, in patients with positive results, it is important to differentiate between transient and persistent infections in order to determine whether follow-up is required. With a DNA-based test, like the HC2 HR HPV test (Qiagen), detection of viral DNA not linked to an active cell infection and cross-hybridization with numerous HPV types not linked to cervical cancer risk means that positive results of DNA tests can lead to overdiagnosis of precancerous abnormalities,8 prompting unnecessary follow-up testing (colposcopy), and treatment.2 Moreover, HPV DNA tests are also likely to provide false-negative results because integration of the viral genome with the host genome over time typically decreases HPV DNA levels as infections progress toward cancer.10 In contrast, RNA levels increase during viral integration because the expression of viral oncogenes escapes viral control.
mRNA-based HPV testing: a needed refinement
A single mRNA-based test, the Hologic Aptima HPV test, has been approved by the FDA in the United States. This test was compared with the test considered to be the current benchmark among the DNA-based assays used for HPV screening, the Qiagen Hybrid Capture 2 test.5,6 In a 2015 study,5 mRNA-based and DNA-based testing in a population of 10,040 women (aged 30 to 60 years) showed statistically similar sensitivities for detecting CIN2+ or CIN3+ lesions. However, the specificity ( In addition to these results, leading experts considered it necessary to obtain long-term data demonstrating the longitudinal negative predictive value of the mRNA test. This data was essential to confirm that the increased interval between screenings proposed for DNA-based testing would also be appropriate for mRNA-based screening. In a 2018 follow-up to the above-cited study, 3,295 triple test-negative women underwent repeat screening a median of six years after their original test.6 In addition, 411 who were test-positive at baseline but were not diagnosed with or treated for precancerous lesions (CIN3) were followed up annually for up to a total of five years (as long as they were test-positive on HPV and/or cytology). The combined follow-up in these triple test-negative and test-positive women identified a total of 28 incident CIN3 cases, of which four were detected in triple test-negative women. The combined cumulative risk of developing high-risk HPV-positive CIN3 over six years was 0.22 percent for women who had tested negative with DNA-based screening and 0.31 percent who had tested negative with mRNA-based screening. This non-significant difference translates into an additional risk of CIN3-positive findings of 0.93 percent per 1,000 test-negative women. The longitudinal relative sensitivity of mRNA-based testing compared with DNA-based testing was 91.5 percent for CIN3+, and the negative predictive values were 99.8 percent for the DNA-based and 99.7 percent for the mRNA-based test. Differences between the two molecular tests were not statistically significant, and the high longitudinal negative predictive values for mRNA-based and DNA-based testing suggest that the two testing modalities will both effectively identify women with low risk of developing high grade precursors or cervical cancer. However, the improved specificity reported with mRNA-based screening in the baseline study suggests that unnecessary follow-up procedures including treatment following a false-positive finding will be less common with the mRNA-based test. In fact, in the original study, 580 women were referred for colposcopy after DNA-based screening compared with 464 who were referred for colposcopy after mRNA-based screening, with no significant difference in the detection of CIN3+. Thus, mRNA-based testing exhibited high sensitivity for identifying women at risk for or with cervical cancer and good longitudinal safety for women who tested negative over a period of at least five to six years. In 2018, the U.S. Preventive Services Task Force observed that false positive findings with unnecessary follow-up testing and treatment are chief harms of cervical cancer screening. Implementation of mRNA-based HPV testing offers an opportunity to reduce unnecessary (and costly) follow-up without increasing the number of women who develop cervical cancer or precancerous conditions after a negative test. Long-term data showing strong negative predictive value with the mRNA-based test are reassuring given the recent introduction of extended screening intervals (more than or equal to three years) in some national cervical cancer screening programs.Conclusion: the role of mRNA-based HPV testing in cervical cancer screening protocols
REFERENCES
genotype specificity of hybrid capture 2. J Clin Microbiol. 2008;46:2595-604.
About the Author