Looking at POCT through a new “value” lens
Advances in technology, combined with the value focus of today’s healthcare system, are changing the how, when, and where of laboratory testing. As part of this shift, these trends are increasing the demand for point-of-care testing (POCT) and broadening the impact that POCT can make in improved patient outcomes and cost savings. Improvements in patient satisfaction also can be realized when laboratory results are made available in real time at the patients’ point of care. In order to utilize POCT to its fullest, however, we have to learn to look at POCT with a different perspective than in the past—through a new “value” lens. We have to carefully determine when and where POCT can have the most benefit and implement IT solutions that ease the complexity of POCT integration and oversight so that the benefits are not overshadowed by the burden of management and integration.
Shifts in testing venues
In its effort to improve population health and efficiency within the U.S. healthcare system, the Affordable Care Act (ACA) launched the beginning of a progression of mergers and acquisitions in which hospitals combine resources with other care facilities to attain the economy of scale necessary to successfully coordinate patient care. For similar reasons, the U.S. healthcare system is experiencing a reduction in inpatient care. In the past, there were loose relationships between hospitals and local ambulatory care centers, but mergers have now created larger consolidated health systems. In addition, physicians are opting for employment rather than ownership in much greater numbers.
These changes in the way healthcare is provided have an effect on how laboratory testing is performed. A decade ago, when physicians were owners, there were clear advantages to lab testing within the office. While there are still many advantages to in-house laboratory testing, when facilities merge, there may be duplicate services. In this situation, logic and economics dictate that testing move to the larger laboratory.
Changes in organizational hierarchy likely influence where lab testing is performed and what testing is needed. For example, when an ambulatory physician’s office is acquired by a hospital, the decision may be made to perform the majority of testing in the hospital lab even if the physician’s office has an internal laboratory. Once the two facilities are under the same financial umbrella, this becomes a question of economy, and often testing will be less expensive in the large hospital lab. However, there may be some testing that the physicians need to have in their office due to turnaround time (TAT) or other efficiencies. Herein lies a perfect opportunity for the expansion of POCT.
The POCT boom
Historically, POCT has been in some ways shunned by the lab because testing tended to be more expensive, less accurate, and a challenge in regard to training and oversight of operators who may be non-laboratorians. The complexities of POCT caused laboratory professionals concern, as many of the details were outside of their direct control.
However, with the changes in healthcare alongside the advances not only to the POCT device technology but in IT systems that can better manage POCT, this outlook is shifting. This is the great POCT boom.
Advances are taking place rapidly in POCT technology, making test results more reliable and testing more simple to perform. There are smaller devices that are capable of much more complex testing than in the past. For example, the U.S. Food and Drug Administration (FDA) recently granted 501(k) clearance to a high-sensitivity cardiac troponin assay that can be used to accurately aid in diagnosis of myocardial infarction in nine minutes.1 POC tests are available to monitor sepsis and iron deficiency, and a hemoglobin A1c test suitable for diagnosis is under FDA review. Molecular POCT is available for influenza A/B, strep, and MRSA. POCT is available for companion diagnostics and personalized medicine, such as the CYP2C19 pharmacogenomic test to determine if patients will respond to Plavix treatment. The rapid rate of POCT development is in response to the need to improve the care that patients receive across the entire care continuum and the need to include the patient as an active member of the care team.
Interoperability and integration
Another huge trend in healthcare has been to leverage health information technology (HIT) to improve care across healthcare organizations. Meaningful Use jump-started broad EMR/EHR implementation, and the push now is for widespread interoperability.
POCT has tremendous potential as a tool to support value-based care, specifically in situations where a rapid TAT can have a profound impact on downstream costs and outcomes. The biggest advantage to POCT is that providing faster access to test results can expedite speed of diagnosis and subsequent treatment. However, this cannot be achieved without electronic integration of POCT results. The benefit of access to advanced POCT devices is diminished if operators are still writing results down on a paper log sheet and data is not immediately accessible to the care team via EHR.
Another concern with POCT in a large integrated healthcare delivery system is that the sheer volume of devices, operators, and locations is almost impossible to manage with spreadsheets and other manual tracking (Figure 1). Just as there have been POCT device advances, there have been IT solutions that can enable remote tracking of POCT needs across multiple locations (QC, devices, training, personnel assessments, etc.).
Lab oversight of POCT
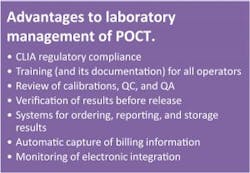
Advancement of POCT is happening in ways that create opportunities to improve care and drive savings. Yet POCT tends to be siloed and often is not managed by the lab. Often, POCT operators do not have a laboratory background, so they may not readily see the reason behind certain seemingly tedious tasks (QC, QA, maintenance, etc.). When POCT falls in with other lab testing and is viewed as an extension of laboratory services, there are specific advantages (Figure 2), and it is more readily accepted that POCT results are included in laboratory interface decisions.2 To meet the evolving needs of healthcare, laboratories are strong candidates for management of POCT. To do so effectively, lab managers who oversee POCT can benefit from a data management and connectivity solution that integrates POCT results into the patient’s chart and eases the challenges of POCT management.
In that context, a crucial factor is to thoughtfully implement POCT in areas where it can be of most benefit—where the TAT can result in downstream savings or the face-to-face interaction promotes a better understanding of the treatment plan, which can lead to an improved outcome. Laboratorians who are invested in increasing their lab’s clinical effectiveness and expanding the lab’s role beyond the laboratory doors should think about the best areas to implement POCT. Once a specific POCT solution has been decided, they should determine how POCT results will be integrated into the EHR and how the POCT program will be monitored (QC, devices, personnel assessments, etc.) (Figure 3).
The POCT “value” lens
It is important during the POCT decision process to consider downstream costs rather than simply comparing POCT costs to core lab costs. We know that the volume of testing in the core lab will typically make the pricing less than POCT. However, if that POCT eliminates an unnecessary hospital admission or readmission, or reduces a hospital length of stay, the downstream savings will far outweigh its costs. This is the new value lens through which we are encouraged to evaluate the need for POCT. Implementing it in the right situations and leveraging HIT to effectively integrate and manage it can increase the lab’s overall value and contribution to patient care.
REFERENCES
- Regulatory roundup: first high-sensitivity troponin test cleared for use in the U.S. Clin Lab News. March 1, 2017. https://www.aacc.org/publications/cln/articles/2017/march/first-high-sensitivity-troponin-test-cleared-for-use-in-the-us.
- Blick KE. The essential role of information management in point-of-care/critical care testing. Clinica Chimica Acta, 2001;307(1-2),159-168. http://dx.doi.org10.1016/S0009-8981(01)00460-0.
Kim Futrell, BS, MT(ASCP), serves as Products Marketing Manager for Orchard Software. Kim has more than 20 years of laboratory management experience. Prior to joining Orchard in 2012, she served as Operations Manager of a multispecialty physician’s office in North Carolina.
About the Author

Kim Futrell, MT (ASCP), MSHI
is the Products Marketing Manager at Orchard Software. Prior to joining Orchard in 2012, Futrell, who has a Master of Science in health informatics, worked as a lab manager for more than 20 years.