Despite multiple studies and thousands of articles in peer-reviewed journals, there remains no consensus regarding benefits provided by vitamin D, beyond maintaining calcium homeostasis and bone health. Nor is there a consensus about the recommended dietary intake (RDI) of vitamin D, optimal serum concentration, advisability of supplementation, or influence of metabolites—or which metabolites should be measured, and with which method. This article is an attempt to provide the most current information regarding these topics.
The hormone precursor, vitamin D3 (cholecalciferol), is primarily obtained through skin exposure to ultraviolet-B (UVB) radiation from sunlight, or through consumption of fatty fish, fish liver oils, beef liver, cheese, and egg yolks. In the United States, foods such as milk and other dairy products, orange juice, and cereal are supplemented with vitamin D3. While the other major hormone precursor, vitamin D2 (ergocalciferol), occurs naturally in mushrooms, minimal concentrations are found in humans unless prescribed, as vitamin D2 is the only form currently available by prescription in the U.S.1 Vitamin D3 is available as a supplement over the counter (OTC) in various forms and concentrations.
Beyond the bones: Additional health benefits?
The possibility that vitamin D might have additional health benefits beyond bone health was raised originally after it was observed that there seemed to be a higher frequency of cancer, cardiovascular disease, and multiple sclerosis in individuals living at higher latitudes, where sun exposure is lower.2 Subsequently, observational studies have shown an association between lower levels of vitamin D and increased risk for chronic diseases such as diabetes, cancer, and cardiovascular disease, suggesting that increased sun exposure at lower latitudes provides beneficial, higher levels of vitamin D3.3 Further studies to determine whether an adequate level of vitamin D is protective against various disorders have been confounded by differences in vitamin D dose, sun exposure, patient adiposity, nutritional status, bolus dosing at intervals versus daily intake, duration of follow-up, and assay variability.3,4
Currently, there have been no completed, large-scale, well-designed, randomized trials that include a racially diverse, initially healthy population. The ongoing Vitamin D and OmegA-3 trial (VITAL) is a 2 X 2 factorial randomized, double blind, placebo-controlled trial designed to address the risks and benefits of taking higher than the recommended dietary allowance (RDA) or RDI of vitamin D3 and/or marine omega-3 fatty acids in the primary prevention of cardiovascular disease (CVD) and cancer.5 This is a U.S. study with a high percentage of African American participants. Recruitment and randomization are completed, and treatment duration will be five years. VITAL is one of four ongoing large-scale worldwide trials, with more than eighty thousand participants collectively, which seek to address whether high doses of vitamin D can impact the primary endpoints of CVD, cancer, and total mortality.
In VITAL, participants receiving vitamin D3 will take 2,000 IU daily. As vitamin D is produced through sun exposure and present in supplemented foods, those in the fatty acid or placebo groups will have some exposure to vitamin D, and there is some concern that 2,000 IU daily will not be sufficient to provide a conclusive difference (personal communication). Ancillary studies looking at diabetes, hypertension, and autoimmune and other disorders are included,5 and initial outcomes are expected in late 2017.3
The most compelling evidence for additional physiologic functions for vitamin D comes from the fact that the bioactive form of vitamin D, calcitriol, [1,25(OH)2D], interacts with a specific nuclear receptor and is transported to the cell nucleus where the vitamin D/vitamin D receptor (VDR) complex interacts with specific DNA sequences, leading to multiple effects. The VDR is present in the human intestines, pancreas, kidney, lung, bone, thymus, spleen, parathyroid, pituitary gland, testis, prostate gland, mammary gland, T and B lymphocytes, and mononuclear cells.2,6 Per Holick, "topical activated vitamin D treatment is the first-line therapy for psoriasis throughout the world," owing to the antiproliferative activity of the active hormone.2 Adequate levels of vitamin D may have a protective effect against the development of multiple sclerosis (MS), and in those who already have MS, may lessen the frequency and severity of symptoms. The risk of developing MS increases the further one lives from the equator.7
RDI and optimal serum concentration
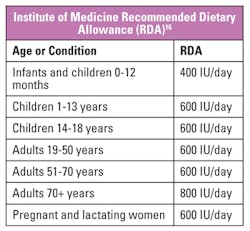
A November 2016 article published in the New England Journal of Medicine highlights the continuing controversy over what level of vitamin D is sufficient. The authors argue that nutrient need, in this case vitamin D, varies, and that the RDA set by the Institute of Medicine (IOM) reflects the "estimated requirement for people at the highest end" of the distribution of the human requirement.8 The authors argue further that "practically everyone in the population (at least 97.5 percent, or within 2 SD of the median) will have a requirement below the RDA," which the IOM has set at 600 IU per day for persons ages one to 70 years, and 800 IU per day for persons over age 70. The article allows that proposed non-skeletal benefits remain under study, and further concludes that many individuals with serum concentrations below 20 ng/mL (50 nmol/L), which the IOM considers generally adequate for bone health, are not necessarily deficient in vitamin D.
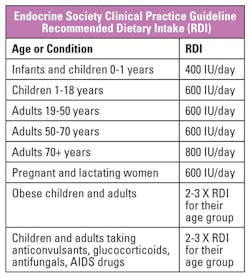
The Endocrine Society Clinical Practice Guideline on vitamin D, published in 2011, is in agreement with the IOM that there is insufficient evidence to recommend screening populations not at risk for vitamin D deficiency. However, the Endocrine Society and the National Kidney Foundation define sufficiency as ≥ 30 ng/mL (74.88 nmol/L).9 The recommended requirements for vitamin D from the IOM and Endocrine Society are similar (Tables 1 and 2), but an understanding of RDA (IOM) versus RDI (Endocrine Society) highlights their different viewpoints regarding vitamin D intake and sufficiency.
Advisability for supplementation
The Endocrine Society Clinical Practice Guideline indicates that unprotected sun exposure is the major source of vitamin D for most humans. But sun exposure is limited by latitude and season, the use of sun screen, and some religious requirements that involve covering the skin; and the ability to produce vitamin D is reduced in deeply pigmented skin and as we age. While the U.S. and some other countries do fortify milk, cereal, and bread, there is controversy as to whether dietary intake and sun exposure are sufficient. Neither the Endocrine Society nor the IOM recommend population screening; however, individuals who have certain diseases or conditions, who are taking certain medications, or who have certain physical traits such as darkly pigmented skin or obesity, should likely be screened, as should older adults at risk for falls or fractures and pregnant or lactating women.8,9 A more complete list of diseases/conditions, medications, and physical traits has been published previously.10
Influence of metabolites
Vitamin D, whether D3 or D2, undergoes two enzymatic hydroxylation steps in the body that result in the formation of the biologically active hormone. Vitamin D is metabolized in the liver to 25-hydroxyvitamin D [25(OH)D], calcidiol, which is the primary storage form of vitamin D and the metabolite that is currently measured to determine sufficiency.2,9 A second hydroxylation step to 1,25-dihydroxyvitamin D [1,25(OH)2D], calcitriol, occurs primarily in the kidney. Vitamin D anabolism and catabolism have been studied extensively, and multiple additional metabolites present at lower concentrations have been described that can be identified and quantified by liquid chromatographic separation.11 The ability to detect these compounds has led to the realization that differences in 25(OH)D recovery among methods may involve metabolite interference.11-13 From a clinical perspective, the ability to identify and quantify these metabolites has led to the discovery that some may have biological effects and/or provide additional clinical information depending on their comparative concentrations to other metabolites.11 For example, 24,25-dihydroxyvitamin D [24,25(OH)2D] is proposed to have biological activity in its own right, the ratio of serum 24,25(OH)2D to 25(OH)D gives information about the response to supplementation, and 24,25(OH)2D may have a role in multiple sclerosis disease progression.14
Which metabolites should be measured and with which method?
According to MÜller and Volmer, 90 percent of vitamin D routine testing is performed using immunoassay techniques.11 These methods are efficient and of lower complexity than chromatographic methods, and vitamin D samples can be included in the overall testing mix, eliminating the requirement for a dedicated platform. However, immunoassay and protein binding techniques only measure total 25(OH)D. Method differences in results related to accuracy and specificity may impact patient care, and have confounded the ability to compare data from different studies and to develop evidence-based guidelines.15 In addition, new studies suggest quantitative information about multiple vitamin D metabolites may be important to fully understand the "pathobiological role and function" of vitamin D.11 The Vitamin D Standardization Program (VDSP), established in 2010, has provided a standardization and certification program with the goal of standardizing all methods to a higher order reference method procedure.15 The vitamin D External Quality Assessment Scheme (DEQAS) and the College of American Pathologists (CAP) both provide accuracy-based proficiency testing programs, and both provide samples containing higher concentrations of 25(OH)D2, which is important for testing patients being supplemented by prescription vitamin D. DEQAS added 24,25(OH)2D to its testing scheme in 2015.
While the IOM advises against overscreening and overprescribing, it is clear that vitamin D testing continues to increase. VITAL and other worldwide trials may eventually provide information as to whether higher doses of vitamin D are beneficial, and assay standardization should provide confidence in the accuracy of the results. As the lack of consensus around the various topics discussed continues, the most compelling hypotheses center on potential differences in vitamin D metabolite profiles and their association in various disease states. Whether vitamin D metabolites are a nuisance in current vitamin D testing or a critical differentiator remains to be determined.
REFERENCES
- Schleicher RL, Sternberg MR, Lacher DA, et al. The vitamin D status of the US population from 1988 to 2010 using standardized serum concentrations of 25-hydroxyvitamin D shows recent modest increases. Am J Clin Nutr. 2016;104:454-461.
- Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers and cardiovascular disease. Am J Clin Nutr. 2004;80 (suppl):1678S-88S.
- Manson JE, Bassuk SS. Vitamin D research and clinical practice: at a crossroads. JAMA. 2015;313:1311-1312.
- LeBlanc ES, Zakher B, Daeges M, et al. Screening for vitamin D deficiency: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;162:109-122.
- Pradhan AD, Manson JE. Update on the Vitamin D and OmegA-3 trial (VITAL). J Steroid Biochem & Molecular Biol. 2016;155:252-256.
- Wang Y, Zhu J, Deluca HF. Where is the vitamin D receptor? Archives of Biochemistry and Biophysics. 2012;523:123-133.
- Weinstock-Guttman B, Zivadinov R, Qu J, et al. Vitamin D metabolites are associated with clinical and MRI outcomes in multiple sclerosis patients. J Neurol Neurosurg Psychiatry. 2011;82:189-195.
- Manson JE, Brannon PM, Rosen CJ, et al. Vitamin D deficiency—is there really a pandemic? NEJM. 2016;375(19):1817-1820.
- Holick MF, Binkley NC, Bishoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2011;96(7):1911-1930.
- Rose AM. Vitamin D testing: clinical and laboratory considerations. MLO. 2013;45(5):8-14.
- Müller MJ, Vomer DA. Mass spectrometric profiling of vitamin D metabolites beyond 25-Hydroxyvitamin D. Clin Chem. 2015;61:1033-1048.
- Carter GD, Jones JC, Shannon J, et al. 25-Hydroxyvitamin D assays: potential interference from other circulating vitamin D metabolites. J Steroid Biochem & Molecular Biol. 2016;164:134-138.
- Cashman KD, Hayes A, Galvin K, et al. Significance of serum 24,25-Dihydroxyvitamin D in the assessment of vitamin D status: a double-edged sword? Clin Chem. 2015;61(4):636-645.
- Swanson JW. Vitamin D and MS: Is there any connection? http://www.mayoclinic.org/diseases-conditions/multiple-sclerosis.
- Sempos CT, Vesper HW, Phinney KW, et al. Vitamin D status as an international issue: National survey and the problem of standardization. Scand J Clin & Lab Invest. 2012;72(243):32-40.
- U.S. Department of Health and Human Services, National Institutes of Health, Office of Dietary Supplements.
Andrea M. Rose, PhD, MBA, serves as Clinical Biochemist and Technical Consultant for Bradenton, Florida-based Gulf Coast ClinLab Consulting, LLC.