Predictability of urinalysis parameters in the diagnosis of urinary tract infection: a case study
ABSTRACT
Early diagnostic strategies to rule out uncomplicated urinary tract infections (UTI) or test of exclusion could significantly improve patient management in addition to providing optimal cost-effectiveness. We evaluated the predictability of dipstick parameters, with particular emphasis on leukocyte esterase (LE) and nitrite (NT) tests and microscopic urine sediment analysis as predictors of urinary tract infection in the setting of an urban university hospital. A total of 9,845 culture positive urine samples (7,095 females, 2,750 males; 8,938 clean catch, 907 catheterized specimens) collected over a period of twelve months from all patients seen at Temple University Hospital, Philadelphia, were included in this retrospective study. Dipstick and urinalysis data were independently correlated and compared with positive culture results. Either individually or in combination, LE and NT were positive in 30% (2,912/9,845), while both LE and NT were negative in 70% (6,933/9,845) of the total culture positive urine samples. There was no correlation of several other measured variables to culture positive urine samples. This study demonstrates that the uses of LE and/or NT are poor screening parameters as predictors of UTI, in the absence of additional clinical information.
INTRODUCTION
Leukocyte esterase (LE, an enzyme produced by neutrophils) and nitrite (NT, the end product of bacterial nitrate reductase acting on nitrate in the urine), two important parameters of dipstick urinalysis, have been frequently used to diagnose UTI. Positive results of LE and NT are often used as a reflex to a urine culture (both in the presence and absence of clinical symptoms of UTI) or, in some cases, even to initiate empiric treatment while the culture results are pending.
There has been an increased understanding in evaluating the clinical usefulness of these diagnostic tests; however, the policy of using LE and NT as tools to guide treatment or to refer for culture has been a topic of considerable debate among clinical microbiologists and clinicians. One former study has shown that a combination of LE, NT, and microscopic examination for bacteria had a sensitivity of 100% for detecting UTI.1 Similarly, studies based on the presence of RBCs2 and microscopic detection of moderate numbers of leukocytes3 have been reported to be related significantly to infection and have a sensitivity of 85% in screening UTI. However, other studies have shown a lack of sensitivity and specificity of these tests as indicators of UTI.4 An additional systematic review of UTI dipstick data concluded that a positive LE or NT test result was the best index or rule-in test, but a negative dipstick result (rule-out test) could not exclude UTI in patients with a high prior probability of contracting the condition.5
In light of the discordance among various studies and paucity of recently reported data, we evaluated the predictability of dipstick parameters, with particular emphasis on LE and NT, and microscopic urine sediment analysis as predictors of UTI in the setting of an urban university hospital.
MATERIALS AND METHODS
Design and setting
A total of 9,845 culture positive urine samples (7,095 females, 2,750 males; 8,938 clean catch, 907 catheterized specimens) collected over a period of twelve months from all patients seen at Temple University Hospital, Philadelphia, PA, were included in this retrospective study.
Urinalysis
The variables measured using urinalysis reagent strips included pH, protein, glucose, bilirubin, specific gravity, blood, ketones, urobilinogen, LE (as an indicator of pyuria), and NT (as an indicator of bacteriuria). Microscopic elements evaluated were RBCs, WBCs, casts, epithelial cells, crystals, bacteria, yeast, and WBC clumps.
Urine culture
The presence of infection in this study was determined by quantitative culture on trypticase soy agar plus 5% sheep blood and MacConkey agar. A colony count of more than 104 organisms/ml (for one or two organisms) was defined as a positive urine culture for clean catch specimens. Full bacterial identification and antimicrobial susceptibility testing were performed for all positive specimens in addition to all isolates from catheterized specimens.6 Specimens that contained more than two isolates (with any quantitation) were considered contaminated and were not included in the analysis. Dipstick and urinalysis data were independently correlated and compared with positive culture results.
Results
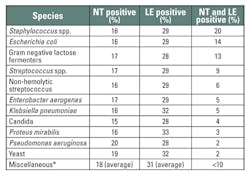
Urinalysis results of the 9,845 culture positive specimens are listed in Table 1. The positive numbers and percentages of NT, LE, protein, and blood respectively are 1,675 (17%), 2,912 (30%), 2,900 (29%), and 3,506 (36%). Of the 9,845 positive cultures, both NT and LE were positive for Staphylococcus spp. in 20% (LE 29%, NT 16%), Escherichia coli in 14% (LE 29%, NT 16%), Gram negative lactose fermenters in 13% (LE 28%, NT 17%), Streptococcus spp. in 9% (LE 29%, NT 17%), non-hemolytic Streptococcus in 6% (LE 29%, NT 16%), Enterobacter aerogenes in 5% (LE 29%, NT 17%), Klebsiella pneumoniae in 5% (LE 32%, NT 16%), Candida in 4% (LE 28%, NT 15%), Proteus mirabilis in 3% (LE 33%, NT 16%), Pseudomonas aeruginosa in 2% (LE 28%, NT 20%), and yeast in 2% (LE 32%, NT 19%). Acinetobacter calcoaceticus-baumanii complex, Aerococcus, alpha and beta hemolytic Streptococcus, Citrobacter, Morganella morganii, Providentia stuartii, Salmonella enteritidis, and Serratia marcescens (“others”) together were <10% (average LE 31%, NT 18%) of the total culture positive results (Table 2). Several other measured variables, including microscopic elements, pH, protein, glucose, bilirubin, specific gravity, blood, ketones, and urobilinogen, showed no correlation to culture positive urine samples.
| Table 1. Results of urinalysis. Data of culture positive specimens (count > 104 CFU/mL) are given as number and percentage. Contaminated samples were not included. |
| * Acinetobacter calcoaceticus-baumanii complex, Aerococcus, alpha and beta hemolytic Streptococcus, Citrobacter, Morganella morganii, Providentia stuartii, Salmonella enteritidis, Serratia marcescens Table 2. Species of nitrite and leukocyte esterase positive cases. |
Discussion
The diagnostic reference standard for UTI infection is quantitative urine culture. However, the issues of cost-effectiveness and processing time in urine culture have prompted the use of other rapid diagnostic strategies to rule out UTI.7 One of the most widely used rapid laboratory diagnostic tools consists of dipstick urinalysis along with microscopic examination of the urine for leukocytes and bacteria; this method is thought by many to be useful in the diagnosis of UTI, especially in symptomatic patients. Various studies of dipstick tests parameters have shown considerable heterogeneity,8 and the results should be interpreted with caution. LE and NT are two frequently assessed parameters in the dipstick analysis of a UTI assessment. They are often used to determine whether treatment is needed or a culture will be performed in cases of a suspected UTI. Many clinicians interpret positive results in these tests as indicators of probable infection and use the results to guide patient treatment.
In the current study of the total 9,845 culture positive urine specimens analyzed, LE was positive in 2,912 specimens (30%). The ability of LE activity to predict significant bacteriuria has been previously demonstrated.9-11 However, LE may render false negative results in the presence of ascorbic acid, boric acid, doxycycline, cefalexin, gentamicin, glycosuria, urobilinogen,12, 13 imipenem, and nitrofurantoin.13 Also, high levels of protein have been shown to inhibit LE detection.9, 12 In women the presence of leukocytes in the urine derived from vaginal contamination could contribute to false positive results associated with UTI.
The NT test is an indirect measure of nitrate-reducing bacteria, including all Enterobacteriaceae, provided the urine contains sufficient dietary nitrate and has been retained in the bladder for longer than four hours.14,15 Performing the test on dilute urine may contribute to false-negative findings.16 Therefore, in patients who may urinate frequently, dilution of LE and NT may result in suboptimal detection. Similar to LE, nitrite results may be affected by common antibiotics, nitrofurantoin, vitamin C, and phenazoperidine.12 The sensitivity of nitrites is thought to vary among different populations; while the test has a high sensitivity in the elderly, the test in pregnant women has the lowest sensitivity.17 It has been reported that NT might be better reflective of UTI in asymptomatic patients and those not on antibiotics.12
In our study, of the total 9,845 culture positive urine specimens analyzed, NT was positive in only 1,675 specimens (17%). This may have been caused by the urine not remaining in the bladder long enough for the organisms to reduce nitrate to nitrite, the patient not having enough dietary nitrate, or reduction of the nitrite to nitrogen or ammonia. This has been supported by findings from other similar studies.11,18,19 Some authors believe that after a positive nitrite test result, empirical therapy should be started, pending results of the urine culture.20 However, based on the results in the present study, NT is not a sufficiently strong predictor of UTI as a sole test. The combination of LE and NT are broadly used, and may be useful only in the initial assessment of bacteriuria. These tests may be falsely negative in UTI with a low colony count, or in recently voided or dilute urine.21
In a systematic review to determine if there was sufficient evidence in the literature to indicate if it was possible to use dipstick tests as a screening process, it was found that the best rule-in test was the LE or NT combination.5 In our study, the group that was NT positive and also positive for LE accounted for 30% (2,912/9,845) of the total culture positive urine samples. It remains to be determined if for NT and LE, both separately or combined, the use of a more stringent definition of infection by increasing the cut-off point of the culture can significantly improve the predictability of NT and LE as indicators of true infection. In use of dipstick analysis, the patient populations and care settings may be factors associated with varying probabilities of the predictability of NT and LE as indicators of UTIs.
It may be expected that the pre-test probability would increase with each level of the healthcare system. While the family physicians may use the dipstick test to diagnose an infection based on clinical signs and symptoms, the hospital-based physicians may order a dipstick test to screen a patient, and then follow up with quantitative culture. Moreover, the dipstick analysis should be performed under optimal laboratory conditions, thereby not affecting the sensitivity, specificity, and the predictive values, unlike those performed under daily practice conditions.22 Interestingly, in some healthcare settings, many laboratories use dipstick testing as part of an algorithm that includes the appearance of the urine, clinical symptoms, and history to determine whether a urine culture needs to be performed. It has been found that a combination of symptom history and dipstick testing (using NT, protein, and hemoglobin) in a wide spectrum of patients identified 89% of infected cases and included 33% of non-infected cases.23
It has been believed that urine dipsticks are useful tools for excluding the diagnosis of UTI based on their high negative predictive values (NPV). Some authors have proposed that urine samples that are visually clear and negative by dipstick testing for blood, protein, NT, and leucocytes could be discarded as “uninfected” based on NPVs of 92% and 98% respectively.24,25 There is disagreement about the quality of urinalysis as a screening test for UTI. While Lohr et al., have shown that a combination of LE, NT, and microscopic examination for bacteria had a sensitivity of 100% for detecting UTI,1 Lenke et al., have demonstrated 100% specificity for the NT test, but only 22% sensitivity for NT.18 However, other studies have demonstrated differing results. In a study by Van Nostrand et al., LE showed a sensitivity of 75% and specificity of 72%; and NT showed a sensitivity of 19.2% and specificity of 94.9%.4 Some studies have shown that dipstick analysis is not sensitive enough to diagnose UTI in high-risk patients.26 Conversely findings of Deville et al.,27 support the concept of using dipstick testing to rule out UTI.
The specific data obtained in this study for NT and LE suggest that the percentage of specimens that were LE positive were generally slightly higher for all organisms evaluated (Table 2) as compared to NT-positive specimens. The percentage of culture positive specimens that were LE-positive was relatively low (approximately 28% to 33%), while the percentage of culture positive specimens that were NT positive was even lower (approximately 15% to 20%). The percentage of culture positive specimens that were both NT and LE positive was also quite low (″20%) and for specific genera was exceedingly low (e.g. yeast, Proteus and Pseudomonas, Table 2).
The present study was based on laboratory findings in a patient population consisting of tertiary care, ambulatory clinic, and family medicine patients. All the culture positive urine specimens (104/CFU) as per the laboratory protocol were included in the study. Some microorganisms such as Enterococcus spp. and Staphylococcus saprophyticus are unable to reduce nitrate to NT. Such cases might have contributed to NT-negative cases, while giving positive culture results. False negative results may occur due to frequent urinations, which lower the exposure of the microorganisms to nitrate; this can also occur with a diet poor in vegetables (a source of nitrates).28 It is widely believed that in the general population, a negative test result for one or both LE and NT tests has a sufficient predictive value to exclude disease, and when both test results are positive, there is sufficient evidence to rule in infection. However, the results of this study suggest otherwise. Care setting, patient population, and symptomatology are the major sources of heterogeneity, and these factors should be taken into account for optimal test use in different clinical circumstances. In part, the discordance in the literature stems from the lack of standardization in the definitions of UTI when associated with bacteriuria.
Conclusion
This study demonstrates that the uses of LT and/or NT in the absence of clinical information are poor screening parameters as predictors of UTI. The urine dipstick test alone does not seem to be useful in all populations to exclude the presence of infection if the results for LE or NT are negative. Indeed, the positive test results have to be confirmed, or pre-test probabilities have to be high on the basis of the clinical history and/or a combination of other tests. The use of LE or NT tests alone to determine the presence of infection may result in unnecessary administration of antimicrobial agents or inappropriate and inaccurate diagnoses. For this reason, culture is still the definitive test to determine whether a urinary tract infection is present. Using culture results will assure that the patient receives the proper antimicrobial therapy or that the patient does not receive unnecessary treatment.
A part of this study was presented at 114th General Meeting of the American Society for Microbiology (Control # 2195; DIVC-20; Specimen Collection, Transportation and Processing), 2012, San Francisco.References
- Lohr JA, Portilla MG, Geuder TG, Dunn ML, Dudley SM. Making a presumptive diagnosis of urinary tract infection by using a urinalysis performed in an on-site laboratory. The Journal of Pediatrics. 1993;122:22-25.
- Wright RA, Euwer R, Scholes EN, Miles SR: Accuracy of standard urinalysis in predicting culture results. Journal of the National Medical Association. 1986;78:43-8.
- Bailey BL, Jr.: Urinalysis predictive of urine culture results. The Journal of Family Practice. 1995;40:45-50.
- Van Nostrand JD, Junkins AD, Bartholdi RK: Poor predictive ability of urinalysis and microscopic examination to detect urinary tract infection. American Journal of Clinical Pathology. 2000;113:709-713.
- Hurlbut TA, 3rd, Littenberg B: The diagnostic accuracy of rapid dipstick tests to predict urinary tract infection. American Journal of Clinical Pathology. 1991;96:582-588.
- McCarter YS,, Hall GS, Zervos M. Laboratory diagnosis of urinary tract infections. Cumitech. Edited by Coordinating ed. SSE. Washington, DC: ASM Press, 2009.
- Lifshitz E, Kramer L: Outpatient urine culture: does collection technique matter? Archives of Internal Medicine. 2000;160:2537-2540.
- Gorelick MH, Shaw KN. Screening tests for urinary tract infection in children: A meta-analysis. Pediatrics.1999;04:e54.
- McNair RD, MacDonald SR, Dooley SL, Peterson LR: Evaluation of the centrifuged and Gram-stained smear, urinalysis, and reagent strip testing to detect asymptomatic bacteriuria in obstetric patients. American Journal of Obstetrics and Gynecology. 2000;182:1076-1079.
- Pels RJ, Bor DH, Woolhandler S, Himmelstein DU, Lawrence RS. Dipstick urinalysis screening of asymptomatic adults for urinary tract disorders. II. Bacteriuria. JAMA.1989;262:1221-1224.
- Zaman Z, Borremans A, Verhaegen J, Verbist L, Blanckaert N. Disappointing dipstick screening for urinary tract infection in hospital inpatients. Journal of Clinical Pathology. 1998;51:471-472.
- Beer JH, Vogt A, Neftel K, Cottagnoud P. False positive results for leucocytes in urine dipstick test with common antibiotics. BMJ. 1996;313:25.
- Stamm WE, Wagner KF, Amsel R, et al. Causes of the acute urethral syndrome in women. NEJM. 1980;303:409-415.
- Evans PJ, Leaker BR, McNabb WR, Lewis RR: Accuracy of reagent strip testing for urinary tract infection in the elderly. Journal of the Royal Society of Medicine. 1991;84:598-599.
- Sussman M. Urinary tract infection: an overview. In: Newall RG, Howell R. (eds.), Clinical Urinalysis. Ames Division, Miles Ltd., Buckinghamshire, UK, pp. 50–61, 1990.
- Pezzlo M. Detection of urinary tract infections by rapid methods. Clinical Microbiology Reviews.1988;1:268-280.
- Patterson TF, Andriole VT. Detection, significance, and therapy of bacteriuria in pregnancy. Update in the managed health care era. Infectious disease clinics of North America. 1997;11:593-608.
- Lenke RR, Van Dorsten JP: The efficacy of the nitrite test and microscopic urinalysis in predicting urine culture results. American Journal of Obstetrics and Gynecology. 1981;140:427-429.
- Loo SY, Scottolini AG, Luangphinith S, Adam AL, Jacobs LD, Mariani AJ: Urine screening strategy employing dipstick analysis and selective culture: an evaluation. American Journal of Clinical Pathology. 1984;81:634-642.
- Koeijers JJ, Kessels AG, Nys S, et al.: Evaluation of the nitrite and leukocyte esterase activity tests for the diagnosis of acute symptomatic urinary tract infection in men. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2007;45:894-896.
- Orenstein R, Wong ES. Urinary tract infections in adults. American Family Physician. 1999;59:1225-1234,1237.
- Winkens R, Nelissen-Arets H, Stobberingh E. Validity of the urine dipslide under daily practice conditions. Family Practice. 2003;20:410-412.
- Dobbs FF, Fleming DM. A simple scoring system for evaluating symptoms, history and urine dipstick testing in the diagnosis of urinary tract infection.The Journal of the Royal College of General Practitioners. 1987;37:100-104.
- Flanagan PG, Rooney PG, Davies EA, Stout RW: Evaluation of four screening tests for bacteriuria in elderly people. Lancet.1989;1:1117-1119.
- Hiscoke C, Yoxall H, Greig D, Lightfoot NF. Validation of a method for the rapid diagnosis of urinary tract infection suitable for use in general practice. The British journal of general practice : the journal of the Royal College of General Practitioners 1990;40:403-405.
- Gomolin IH, McCue JD. Urinary tract infection in the elderly patient. Infect Urol. 2000;13(5a).
- Deville WL, Yzermans JC, van Duijn NP, Bezemer PD, van der Windt DA, Bouter LM. The urine dipstick test useful to rule out infections: a meta-analysis of the accuracy. BMC Urology. 2004;(4):4.
- Dos Santos JC, Weber LP, Perez LR: Evaluation of urinalysis parameters to predict urinary-tract infection. The Brazilian journal of infectious diseases:an official publication of the Brazilian Society of Infectious Diseases. 2007;11:479-481.