The key to controlling sexually transmitted infections: Early diagnosis
Sexually transmitted infections (STIs) are surging worldwide, posing a significant public health threat. The consequences of delayed diagnosis range from individual health complications to increased transmission rates, and even antibiotic resistance. Yet, many STIs remain underdiagnosed due to their asymptomatic nature. Let’s explore the critical importance of early diagnosis, the rise in STI cases, and the latest advancements in diagnostic technologies available to curb the rise of infection.
The growing STI crisis
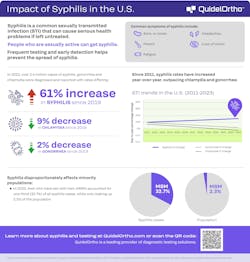
Fueling the STI crisis is the number of different infectious diseases, with syphilis, gonorrhea, chlamydia, and trichomoniasis in the lead. In the United States alone, the Centers for Disease Control and Prevention (CDC) reported over 2.5 million cases of STIs in 2022, with congenital syphilis cases increasing by 32% in just one year.1
Globally, the numbers are just as staggering — in the United Kingdom, syphilis and drug-resistant gonorrhea have reached record levels, with syphilis cases increasing nearly 10% year over year.2 Similarly, Australia has seen a decade-long climb in chlamydia and gonorrhea infections, with chlamydia as the most commonly reported communicable disease.3 These alarming trends make early diagnosis more critical than ever.
Why early diagnosis matters
Early diagnosis for STIs is crucial for several reasons. First, earlier and faster treatment leads to a decrease in transmission. The sooner an STI is diagnosed, the quicker treatment can begin, reducing transmission and breaking infection chains. Second, early diagnosis can prevent severe complications. Untreated, STIs can lead to infertility, miscarriage, chronic pain and increased susceptibility to human immunodeficiency virus (HIV). Chlamydia and gonorrhea, for example, often go unnoticed until they cause irreversible reproductive damage.3 In the case of syphilis, untreated infection can lead to irreversible organ damage to the heart, the eyes, and the brain, which can be life-threatening. Third, early diagnosis can curb antibiotic resistance. Rapid diagnosis ensures proper treatment, helping prevent the misuse of antibiotics that can fuel drug-resistant strains of STIs.2
Asymptomatic infections: The challenge
Controlling STIs has its obstacles, as they’re known to be stealthy. Many infections remain without symptoms for months — or even years — before manifesting. For example, gonorrhea often presents no symptoms in women, which increases the risk of unknowingly spreading the disease.1 Human papillomavirus (HPV) is another example, with most cases clearing on their own while a few develop into cervical cancer. Syphilis commonly enters a latent stage, which can last for years without any symptoms, often leading a person to believe the infection has cleared. Without regular screening, these hidden infections can cause serious health crises.1
Advancing STI diagnosis
The response to the STI crisis continues to evolve with cutting-edge diagnostic advancements, for example:
- At-home testing kits: Australia has approved at-home gonorrhea and chlamydia tests that deliver results in just 15 minutes. These kits allow individuals to take testing into their own hands, providing privacy and accessibility, reducing the barriers to testing.3
- Rapid testing: Rapid STI testing provides results quickly, allowing immediate treatment decisions and limiting transmission risks.2
- Molecular diagnostics: Advanced molecular techniques can detect infections earlier, including in asymptomatic patients, facilitating early and accurate diagnosis.4
The ways public health can help control STIs
There are several public health strategies that can help control the rise in STIs. Through comprehensive sexual education, public health agencies can encourage awareness, which is the first step in prevention. Education programs must emphasize the importance of regular testing and safe practices. Public health agencies should prioritize affordable, accessible testing services, including self-testing kits, to create wider access to testing. Implementing routine screening protocols, including STI screening, especially for high-risk groups, can help reduce undiagnosed cases.1 Public health agencies can also create and advocate for confidential systems for notifying and treating partners to help break the cycle of reinfection.5 Finally, public health agencies should continue to invest in the development of new diagnostic tools and treatments.1
Of all the available strategies to control and manage the rise of STIs worldwide, early diagnosis is the key. It helps facilitate rapid treatment, reduces transmission and prevents severe health consequences. As STI rates continue to climb, leveraging the latest diagnostic innovations, increasing awareness and expanding testing access will be vital to curbing this public health crisis.
References
- CDC. Sexually transmitted infections surveillance, 2023. STI Statistics. November 12, 2024. Accessed April 22, 2025. https://www.cdc.gov/sti-statistics/annual/index.html.
- Li L. Tracking—and tackling—the recent resurgence of syphilis. Healthcare Business Today. November 10, 2024. Accessed April 22, 2025. https://www.healthcarebusinesstoday.com/resurgence-syphilis-tracking-tackling/.
- QuidelOrtho. Chlamydia: A silent threat. Published 2023. Accessed April 22, 2025. https://www.quidelortho.com/global/en/resources/diseases-conditions/sexually-transmitted-infections/chlamydia.
- QuidelOrtho. Cytomegalovirus and its implications. Published 2023. Accessed April 22, 2025. https://www.quidelortho.com/global/en/resources/diseases-conditions/herpes-related-diseases/cytomegalovirus.
- QuidelOrtho. Understanding trichomoniasis: The overlooked STI. Published 2023. Accessed April 22, 2025. https://www.quidelortho.com/global/en/resources/diseases-conditions/sexually-transmitted-infections/trichomoniasis.
About the Author

Lily Li, MD, PhD, MBA
is the Medical Safety Officer and Senior Director, Medical, Scientific & Clinical Affairs at QuidelOrtho, a global leader in in-vitro diagnostics.