Different approaches to SARS-CoV-2 testing using mass spectrometry
Current detection methodologies for SARS-CoV-2 include molecular testing using real-time, reverse transcription polymerase chain reaction (RT-PCR) (gold standard), or a variety of other amplification-based methods, as well as antigen testing by a variety of immunoassay-based methodologies. Two different mass spectrometry-based methodologies/technologies, will be discussed: matrix assisted laser desorption ionization – time of flight (MALDI-ToF) and liquid chromatography – tandem mass spectrometry (LC-MS/MS). These methods are used for the detection of SARS-CoV-2 nucleic acid (molecular) or protein molecules (antigen).
Mass spectrometry-based testing for SARS-CoV-2
Mass spectrometry-based technologies for COVID-19 testing detect cDNA from SARS-CoV-2 RNA or peptides derived from SARS-CoV-2 proteins. With these methodologies, ideal target candidate viral cDNA or peptides have previously been identified for targeted analysis. Samples are collected and prepared by either RT-PCR or protein digestion as appropriate. The cDNA (currently analyzed by MALDI-ToF) or peptides (currently analyzed by LC-MS/MS) from the sample are then ionized and introduced into the mass spectrometer, where they are detected and analyzed. It is generally accepted that more than one SARS-CoV-2 target region has to be positive for the mass spectrometry assay to be positive.
MALDI-ToF mass spectrometry testing for SARS-CoV-2
MALDI-ToF mass spectrometry is not new to the clinical laboratory. It has been approved for use by the U.S. Food and Drug Administration (FDA) as a bacterial identification mass spectrometry-based diagnostic test for several years. This technology combines ionization of sample molecules by MALDI with a ToF analyzer to identify the molecules of interest.
Currently (as of June 22, 2021), there are three (two are laboratory restricted) mass spectrometry-based tests for SARS-CoV-2 detection with emergency use authorization (EUA) from the FDA.1 All three testing methodologies are based on a multiplex RT-PCR amplification of SARS-CoV-2 nucleic acids from upper respiratory tract specimens followed by MALDI-ToF mass spectrometry analysis for qualitative detection.
All three of the FDA EUA approved tests also use the same nucleic acid amplification methodology and panel kit for SARS-CoV-2 RNA detection. Prior to mass spectrometry detection, RNA is isolated from upper respiratory samples, converted into cDNA, and specific gene regions are amplified by RT-PCR. In this instance, the specific regions amplified for SARS-CoV-2 testing are regions corresponding to the nucleocapsid gene, open reading frame (ORF)1 and ORF1 ab. Post RT-PCR, excess dNTPs are inactivated before another round of PCR amplification is performed, adding one additional nucleotide to a sequence specific probe bound to the amplified SARS-CoV-2 target region. This generates allele-specific PCR products with different specific masses.
After SARS-CoV-2 targeted regions have been amplified and probe added, MALDI-ToF mass spectrometry is used to detect and determine the masses of the amplified PCR product(s). With this type of mass spectrometer, molecules are ionized by MALDI, then analyzed by ToF. MALDI is an ionization technique that uses matrix added to samples and a nitrogen laser to ionize (acquire a charge) and vaporize samples spotted onto a sample plate. The ionized sample then travels down the flight tube of the mass spectrometer, where the different PCR products’ time of travel is related to its mass to charge ratio (m/z), with heavier ions taking longer to reach the detector. The information resulting from this analysis generates a graph (mass spectrum), plotting m/z on the x-axis and relative abundance on the y-axis. The specificity is obtained from the m/z of the ion and allows for the identification of previously determined SARS-CoV-2 RNA targets being identified in the sample.
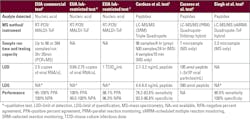
The targeted cDNA regions tested by the three EUA approved tests contain a panel of five SARS-CoV-2 target assays to remain robust in the presence of novel mutations. The commercially available EUA SARS-CoV-2 test can run 96 to 384 samples at one time. The PCR amplification steps takes about 2.75 hours, depending on thermocycler performance, while the time to analyze 384 samples by mass spectrometry is about 50 minutes. This test also reports a limit of detection (LOD) from nasopharyngeal swab samples to be 2.5 copies/µL with a positive percent agreement (PPA) of 95-100% and negative percent agreement (NPA) of 100%.2 Similar performance characteristics of the other two laboratory-restricted EUA tests are listed in Table 1.
LC-MS/MS Testing for SARS-CoV-2
While there currently is no mass spectrometry-based method for SARS-CoV-2 testing approved by the FDA (EUA or otherwise) other than the previously mentioned MALDI-ToF tests, there are several LC-MS/MS based methodologies for SARS-CoV-2 testing reported in the literature. This technology differs from MALDI-ToF in several ways. First, it tends to be a targeted proteomics approach, allowing for both qualitative and quantitative analysis using tryptic-digested peptides from SARS-CoV-2 proteins as the analytical target (although other targets can also be analyzed). In addition, molecules are first separated using LC before introduction into the mass spectrometer. Also, the mass spectrometers typically used in this methodology combine ionization of sample molecules by either electrospray ionization (ESI) or atmospheric pressure chemical ionization (APCI) with a triple quadrupole mass analyzer (or higher-end hybrid) to identify the molecules of interest. Another way the mass spectrometry methodology differs is that LC-MS/MS uses a targeted approach, such as selected reaction monitoring (SRM) or other closely related methods, where only selected peptides from digested SARS-CoV-2 proteins in a sample are first filtered and “isolated” by the mass spectrometer based on their m/z, targeted for fragmentation, then only specific fragment product ions are detected and analyzed either qualitatively or quantitatively. Of note, if an unknown mutation is present in the targeted peptide, the m/z will differ, and it will not be detected.
The targeted proteomics methodologies are still more research-based, versus clinically adopted methods. They tend to utilize higher-end instrumentation; although, laboratories also utilize the more clinically available instrument, a triple quadrupole. LC-MS/MS methodologies are typically more complex than a basic MALDI-ToF assay with a higher level of method understanding and user expertise needed to develop/run the test. However, laboratories that typically run mass spectrometry-based tests, such as drugs of abuse, steroid analysis, or vitamin D assays, are familiar with most of this technology. Laboratories can also reduce testing complexity (and turnaround time) by utilizing automated instrumentation on the front end for sample handling and processing, with automated data analysis on the back end.
Select examples from the literature using this methodology demonstrate the feasibility of this method for use as a clinical diagnostic assay, including the method by Cardozo using an SRM approach and targeting two SARS-CoV-2 peptides from nucleoprotein.3 Cazares uses parallel reaction monitoring (PRM) for a proof-of-principal demonstration using two peptides from the spike protein and two peptides from the nucleoprotein.4 Singh targets two SARS-CoV-2 peptides, one from the spike protein and one from the replicase polyprotein 1ab protein.5
Some of these assays report running up to 500 samples per day.3 Others demonstrate a LOD of 195 amol of peptide and LOQ of 390 amol of peptide.4 The authors estimated that the LOD is equivalent to approximately 2x105 viral particles/mL, which is only 2 to 20 times higher than the lowest range of the observed SARS-CoV-2 titer from saliva (1x105 to 1x1011 copies/mL) and nasal (1x104 to 1x1010 copies/mL) swab samples,4 and a factor of ten greater than the commercially available EUA mass spectrometry method. Moreover, they also state sample handling was not optimized and could have impacted detection.4 Unlike in RT-PCR, proteins cannot be exponentially multiplied; therefore, sensitivity can be lower when compared to this method. However, higher-end mass spectrometers can detect very low quantities of peptides, some in the low amol range, which may compensate for the lack of amplification. Sensitivity using LC-MS/MS methods have been reported in the 78.2% to 90.5% range and specificity in the 93.3% to 100% range.3,5 Table 1.
Conclusion
There are many different approaches that can be taken for mass spectrometry-based SARS-CoV-2 testing. Currently, only three different companies/laboratories using the RT-PCR/MALDI-ToF methodology have EUAs for SARS-CoV-2 testing. These RT-PCR/MALDI-ToF tests detect the genetic component of SARS-CoV-2, while the LC-MS/MS based methodologies tend to detect the protein (or antigen) component of SARS-CoV-2 by targeted proteomics. In the case of RT-PCR/MALDI-ToF, the mass spectrometer is used to detect the amplified nucleic acid product. With the LC-MS/MS method, mass spectrometry is integral to the methodology itself.
References
- U.S. Food and Drug Administration. In vitro diagnostics EUAs - molecular diagnostic tests for SARS-CoV-2. https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/in-vitro-diagnostics-euas-molecular-diagnostic-tests-sars-cov-2. Accessed June 22, 2021.
- U.S. Food and Drug Administration. MassARRAY SARS-CoV-2 Panel Instructions for Use. https://www.fda.gov/media/143334/download. Published May 3, 2021. Accessed July 12, 2021.
- Cardozo KHM, Lebkuchen A, Okai GG, et al. Establishing a mass spectrometry-based system for rapid detection of SARS-CoV-2 in large clinical sample cohorts. Nat Commun. 2020;11, 6201. https://doi.org/10.1038/s41467-020-19925-0.
- Cazares LH, Chaerkady R, Samuel Weng SH, et al. Development of a parallel reaction monitoring mass spectrometry assay for the detection of SARS-CoV-2 spike glycoprotein and nucleoprotein. Anal Chem. 2020;92(20):13813-13821. doi: 10.1021/acs.analchem.0c02288. Epub 2020 Oct 5. PMID: 32966064; PMCID: PMC7537550.
- Singh P, Chakraborty R, Marwal R, et al. A rapid and sensitive method to detect SARS-CoV-2 virus using targeted-mass spectrometry. J Proteins Proteom. 2020;Aug 31:1-7. doi: 10.1007/s42485-020-00044-9. Epub ahead of print. PMID: 33132628; PMCID: PMC7457902.
- U.S. Food and Drug Administration. Emergency Use Authorization (EUA) summary SARS-CoV-2 Massarray Test (National Jewish Health Advanced Diagnostics Laboratory). https://www.fda.gov/media/142548/download. Published September 9, 2020. Accessed July 12, 2021
- U.S. Food and Drug Administration (FDA) Emergency Use Authorization (EUA) summary Ethos Laboratories SARS-CoV-2 MALDI-ToF Assay (Ethos Laboratories). https://www.fda.gov/media/140780/download. Published September 21, 2020. Accessed July 12, 2021.
About the Author

Leann M. Mikesh, PhD
serves as an Adjunct Assistant Professor and instructor of the clinical mass spectrometry course series in the Biomedical Laboratory Diagnostics Program at Michigan State University.