In a recent decision memo, the Centers for Medicare and Medicaid Services (CMS) outlined the criteria that will determine if it will pay for next-generation sequencing (NGS) tests for patients with inherited ovarian or breast cancer.
The agency’s decision specified that CMS will pay for NGS tests if a patient’s case meets these criteria:
- A diagnosis of ovarian or breast cancer
- A clinical indication for hereditary breast or ovarian cancer
- A risk factor for hereditary breast or ovarian cancer
- If the patient had not been previously tested using the same germline NGS test for the same genetic content.
Even if these criteria are met, the agency says it will only pay for laboratory tests using NGS that have been approved or cleared by the Food and Drug Administration (FDA) and that are performed in CLIA-certified labs. CMS also said the results of the tests should point physicians to targeted treatments for their patients.
However, CMS left open the door to broader reimbursement of NGS sequencing tests by saying that local Medicare Administrative Contractors (MACs), which are private insurers that adjudicate claims for CMS, have the authority to relax some of the payment standards. CMS said MACs can approve payment for NGS tests for any inherited cancer that also meets the other conditions CMS outlined. The agency also said MACs can approve tests that do not have FDA approval or clearance if they are performed in a CLIA-certified lab.
In addition, MACs may determine whether to cover NGS tests for RNA sequencing and protein analysis testing. CMS officials also note in the memo that the agency will continue to pay for diagnostic tests using NGS for “beneficiaries with recurrent, relapsed, refractory, metastatic, and/or advanced stage III or IV cancer.”
In announcing the decision, CMS Administrator Seema Verma said, “We recognize that cancer patients shoulder a heavy burden, so we’re leaving no stone unturned in supporting women’s health and getting all patients the care they need. NGS testing provides clinically valuable information to guide patients and physicians in developing a personalized treatment plan.”
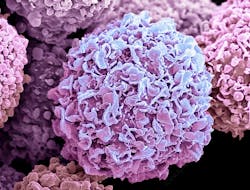
The agency also wants to give patients more opportunities to personalize their cancer care, CMS said in a news release announcing the decision. Genetic tests can give patients a more complete profile of their cancer cells and may help identify proven, targeted treatments. Patients who use NGS tests may also find they are good candidates for cancer clinical trials.
In the decision memo, CMS noted that it outlined the situations in which MACs could broaden access to the NGS tests to “offer a degree of flexibility as new evidence is collected without having to reconsider each time.”
Decision memo timeline
When CMS issued its first national payment policy for tests using NGS in 2018, it approved test payments only “for patients with recurrent, relapsed, refractory, metastatic or advanced cancers.” Bowing to industry pressure, the agency reopened discussions about its reimbursement policy in 2019, beginning with an initial 30-day comment period.
After analyzing 82 comments, CMS issued a proposed decision memo in October 2019, which prompted 43 stakeholders to file comments. In January 2020, CMS issued the final decision memo that allows reimbursement for all stages of breast and ovarian cancer.
Broader payment criteria
As part of the decision memo, CMS officials noted that some commenters pointed out that there currently are no FDA-approved or -cleared NGS tests for inherited cancer on the market.
Commenters also had other objections to CMS’ reimbursement policy. For example, in its written comments, the American College of Clinical Pathology (ACCP) urged CMS to approve coverage of NGS tests nationally for women who have not been diagnosed with ovarian or breast cancer but are at increased risk of developing those diseases.
In these cases, the tests are “important to identify certain genetic markers that aid with the early detection of cancer,” Matthew Schulze, director of the Center for Public Policy at the ACCP, wrote. Women with ovarian cancer, in particular, are not usually diagnosed until the disease has reached advanced stages, Schulze said.
The ACCP also urged CMS to extend national coverage to laboratory-developed tests (LDTs) that use NGS. “LDTs are increasingly being integrated into standard practice for diagnosing and managing disease, predicting the risk of developing disease, and informing decisions about lifestyle and behavior—particularly molecular genetic tests for which there are few commercial tests available,” Schulze wrote.