Health information technology can support population health management
The United States healthcare system continues to shift its focus toward outcome improvements, and that makes it prudent for healthcare professionals to look at the broader picture of health and address care needs for populations as well as individuals. At the same time, health information technology (HIT) is becoming more widely used to improve patient care, and such technology is essential for broad population health management (PHM).
Today’s population health management
Healthcare organizations (HCOs) use PHM to identify and stratify their specific patients into groups by diagnoses and other relevant patient data to proactively determine the most appropriate interventions. PHM can take place on a small scale or can be global. A comprehensive PHM plan will address patient needs at all levels—from high-risk to healthy patients who can benefit from preventive care.
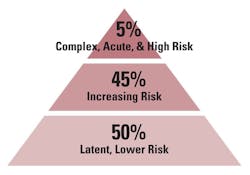
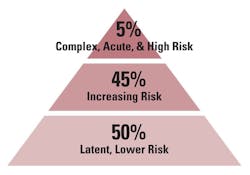
The first step in PHM is to use data to risk-stratify the patient population into groups according to health categories and care needs. If a patient population is represented in a pyramid (Figure 1), typically the largest, bottom portion of the pyramid will be the healthy patients who need preventive services depending on gender, age, and so on. This low-risk group is typically approximately 50 percent of the population and accounts for only about eight percent of healthcare costs.1 The goal of a PHM program is to keep these patients healthy and in the low-risk category. In the middle tier are the mid- or rising-risk patients who need appropriate care to keep them from rising to the top tier, where the sickest patients are represented. The top tier includes high-risk patients with multiple co-morbidities. This five percent of patients can account for up to 50 percent of healthcare costs.1 Therefore, the high-risk tier is often an initial target for a PHM program.
Predictive modeling and care team interventions
Once a patient population is risk-stratified, predictive modeling algorithms can be used to predict future health status. Predictive modeling is helpful in determining appropriate preventive measures and early interventions. Performance of predictive modeling requires computer algorithms capable of recognizing patterns in patient data and forecasting the likelihood of patients developing certain conditions.
Grouping patients into logical segments based on age, condition, risk, etc., allows providers and care teams to develop appropriate interventions for each group and each patient. Care managers then actively manage patient cases, from preventive care reminders such as mammograms for women over 40 to working with Meals on Wheels to deliver healthy meals to home-bound patients.
HIT aspects
A key element in a PHM program is the effective use of HIT tools to identify and stratify patient groups, generate alerts or messages that communicate with providers and patients, and perform follow-up metrics to analyze progress. An EMR/EHR is an integral part of a PHM endeavor, but it takes other HIT tools and data analysis for a comprehensive PHM effort.
Lab & claims data. Although PHM is expected to become widespread, many HCOs are in the beginning stages of PHM, using the HIT tools they have available to begin leveraging their patient data to improve care. As a first step, PHM efforts start with claims, lab, and electronic health records (EHR) data being used to perform risk analyses and identify patients who need follow-up care.
Disease registries. Electronic registries, fed by EHR and administrative data, are another source of actionable data and risk stratification reports. There are benchmark registries that allow HCOs to measure care plan effectiveness for certain conditions (e.g., heart disease, diabetes) compared to national averages. When registries are coupled with evidence-based clinical protocols, specially designed applications can generate messages to patients to trigger appointments for necessary chronic and preventive care. Care managers use this information to follow up with patients after discharge.
Data warehouses. Large HCOs and integrated delivery networks (IDNs) use data warehouses to aggregate data from multiple sources, including clinical and claims data and patient registries. For example, a six-hospital network in New Jersey uses Cerner’s HealtheIntent tool to support a data warehouse that compiles data from 20 disparate sources, including: a disease registry; systems from hospitals, clinical, long-term care facilities, home health, lab, and payers; and the local health information exchange (HIE).2 The data warehouse houses more than 250,000 disease registries and stratifies more than a million patients to identify and prioritize care gaps.2
Health information exchanges & patient portals. HIEs that can share patient data across HCOs and geographical areas can be beneficial to a large-scale PHM program. With comprehensive data available, providers can access patient information in real time to improve clinical decision making at the point of care. As an example, the Medical Society of New Jersey offers a state HIE—One Health New Jersey—that includes “patient portal access, health data analytics tools, and population health management capabilities.”3 TriCore, which is the largest laboratory in New Mexico, is participating in PHM by creating physician and patient portals that are intended to compile lab data from various HCOs across the area into one “community-based longitudinal record.”4
Telehealth & mobile health apps. Telehealth and mobile health apps are a fast-growing area of healthcare that helps address access issues and increase mobility for patients and providers. Growth in this area of HIT is rapidly expanding and can be a vital tool for a PHM program. Home telehealth devices, health trackers, and other mobile apps can transmit data to a care manager to support ongoing monitoring. For example, the Veterans Health Administration’s telehealth program reduced hospital admissions by 19 percent and length of stay (LOS) by 25 percent.5
Laboratory involvement in PHM
Laboratories need to understand and find ways to embrace value-based reimbursement and PHM to thrive in the evolving healthcare environment. Avoidable hospital admissions, unnecessary readmissions, and reducing hospital LOS add up to large savings.
A great deal of the data used for PHM comes from the laboratory, creating opportunities for the lab to demonstrate its value by being involved in and supportive of PHM efforts. The laboratory can be involved, for example, by making sure test results that indicate a care manager is needed are communicated promptly.
A pinnacle PHM goal is to be able to provide evidence-based data to the provider or care team member at the point of care to identify care gaps and inform decision-making in a real-time manner. Laboratory professionals can assist in the development of specific disease order sets and EHR alerts that provide the most value.
The laboratory is a key ancillary with a large amount of data that can be incorporated into PHM, and laboratory professionals have an in-depth understanding of lab orders and results that can be of value to a PHM team. With a comparable understanding of PHM, the lab can play a proactive role in communicating results and coordinating care. This will involve laboratory professionals taking the initiative to determine how their laboratory can contribute to PHM and providing their expertise where it can benefit patient care.
REFERENCES
- Sullivan P. 5 percent of Medicaid patients account for half of program’s costs. The Hill. May 8, 2015. http://thehill.com/policy/healthcare/241491-5-percent-of-medicaid-patients-account-for-50-percent-of-costs.
- Siwicki B. Healthcare providers driving population health with data, mobile apps, telehealth tools. Healthcare IT News. March 15, 2016. http://www.healthcareitnews.com/news/healthcare-providers-driving-population-health-data-mobile-apps-telehealth-tools?
- Monica K. NJ Medical group starts physician-led health information exchange. EHR Intelligence. December 13, 2017. https://ehrintelligence.com/news/nj-medical-group-starts-physician-led-health-information-exchange.
- Versel N. Dominant N.M. lab seeks active role in population health. Clinical Innovation + Technology. February 19, 2015. http://www.clinical-innovation.com/topics/analytics-quality/dominant-nm-lab-seeks-active-role-population-health.
- Dinesen B, Nonnecke B, Lindeman D, et al. Personalized telehealth in the future: a global research agenda. J Med Internet Res. 2016:18(3):e53.
Kim Futrell, MT(ASCP), MSHI, serves as Products Marketing Manager and Regulatory Affairs Officer for Orchard Software. In her role she is an advocate for laboratories, lab informatics, and Orchard’s laboratory information system software products.
About the Author

Kim Futrell, MT (ASCP), MSHI
is the Products Marketing Manager at Orchard Software. Prior to joining Orchard in 2012, Futrell, who has a Master of Science in health informatics, worked as a lab manager for more than 20 years.